Local & Regional Anesthesia for Eye Surgery
--- Authors: Jacques Ripart, MD; Kenneth Mehrige, MD; Robert Della Rocca, MD
|
Introduction Ophthalmic surgery is one of the most frequent surgical procedures requiring anesthesia in developed countries.(1) Perioperative morbidity and mortality rates associated with eye (eg, cataract) surgery are low.(2,3) Nevertheless, because patients with cataracts tend to be older and to have serious comorbidities,(4–9) systematic preoperative evaluation should be performed to consider a patient eligible for surgery.(9) Anesthetic management may contribute to the success or failure of ophthalmic surgery. A closed-claims analysis by Gild and coworkers(10) found that 30% of eye injury claims associated with anesthesiawere characterized by the patient moving during ophthalmic surgery. Clinical strategies to ensure patient immobility are essential, as blindness is the outcome in many cases of eye injury. Most problems occurred during general anesthesia. Quicker patient rehabilitation and fewer complications are the main reasons why many ophthalmic surgeons are choosing local (LA) over general anesthesia.(11–13) In the past, regional anesthesia on the eye typically consisted of retrobulbar anesthesia (RBA), with the surgeon performing the block. Widespread use of the phacoemulsification technique, however, has changed the anesthesia requirements for this technique; total akinesia and lowered intraocular pressure are no longer necessary. Consequently, conventional RBA is used less frequently today, particularly since it carries a greater risk for complications than do the emerging techniques. The newer techniques do not provide akinesia of the globe paralleling that of the retrobulbar block; however, they are useful for anterior segment surgery, especially cataract surgery. Accurate knowledge of anatomy and of various anesthetic techniques are necessary to determine the appropriate block for specific clinical situations. This chapter will review the relevant anatomy of the eye, classic (retro and peribulbar) needle block techniques, emerging anesthesia techniques, and choice of LAs and adjuvant agents. Anatomy
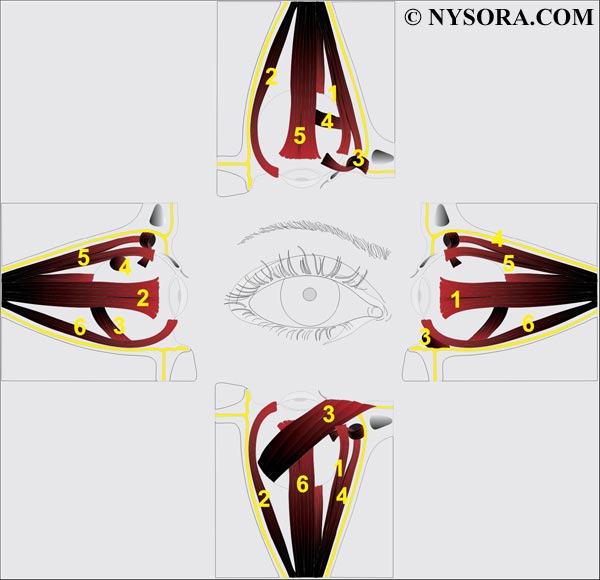
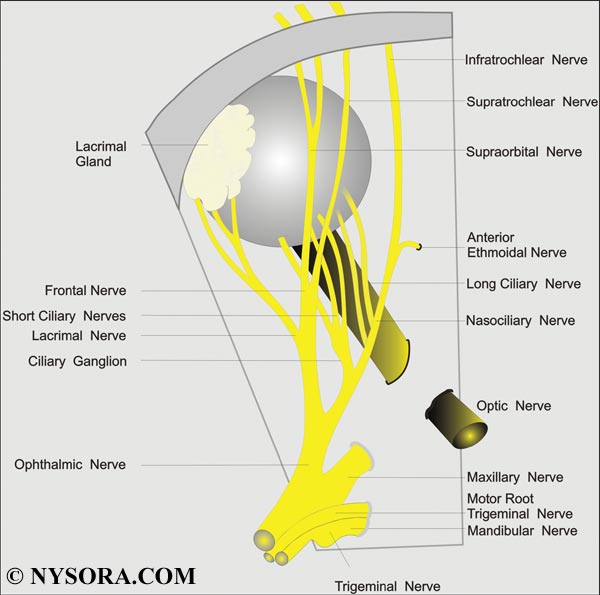
The cavity of the orbit has a truncated pyramid shape, with a posterior apex, and a base corresponding to the anterior aperture. The orbit contains mainly adipose tissue, and the globe is suspended in the anterior part. The four rectusmuscles of the eye insert anteriorly near the equator of the globe (Figure 1). Posteriorly, they insert together at the apex on the tendineus anulus communis of Zinn, through which the optic nerve enters the orbit. The four rectus muscles delineate the retrobulbar cone, which is not sealed by any intermuscular membrane.(14–17) Sensory innervation is supplied by the ophthalmic nerve (first branch of the trigeminal nerve [V]), which passes through the muscular cone (Figure 2). The trochlear nerve (IV) provides motor control to the superior obliquemuscles, the abducens nerve (VI) to the lateral rectus muscle, and the oculomotor nerve (III) to all other extraocular muscles. All but the trochlear nerve pass through the muscular conus. Injection of LA solution inside the cone will provide anesthesia and akinesia of the globe and the extraocular muscles. Only the motor nerve to the orbicularis muscle of the eyelids has an extraorbital course, coming from the superior branch of the facial nerve (VII). Many major structures are located within the muscular conus and are, therefore, at risk of needle and injection injury. These include the optic nerve with its meningeal coverings; blood vessels of the orbit; and the autonomic, sensory, and motor innervation of the globe. For this reason, some authors advise that introduction of the needle into the muscular cone be avoided and suggest that needle insertion be limited to the extraconal space.(18,19) However, the extraconal space is only a virtual space, because the rectus muscles are in contact with the bone walls of the orbit. The scleral portion of the globe is surrounded by Tenon's capsule, a fibroelastic layer stretching from the corneal limbus anteriorly to the optic nerve posteriorly. Its proper anatomic name is the facial sheath of the eyeball. It delimits a potential space named the episcleral space (sub-Tenon's space). This is only a virtual space that expands when fluid is injected into it. Retrobulbar Anesthesia 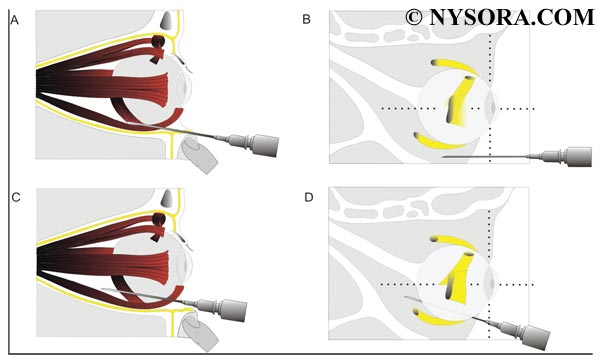
Figure 3: Retrobulbar anesthesia. The needle is introduced through the skin below the inferior lid at the junction between the lateral third and the medial two thirds of the inferior orbital edge. Historically, RBA has been the gold standard for anesthesia of the eye and orbit. This technique generally consists of injecting a small volume of LA solution (3-5 mL) inside the muscular cone (Figure 3). A facial nerve block is occasionally required to prevent blinking. Because of its extraconal motor control, the superior oblique muscle may frequently remain functional, precluding total akinesia of the globe. The main hazard of RBA is risk of injury to the globe or to one of the anatomic structures in the muscular cone. Near the apex, these structures are packed in a very small space and are fixed by the tendon of Zinn, which prevents them from moving away from a needle. The resulting potential complications are detailed later. Conventional Technique Since its formal description by Atkinson toward the end of the nineteenth century,(20) conventional RBA has not changed for decades. The patient is asked to look in the "up-and-in" direction. The needle is introduced through the skin below the inferior lid at the junction between the lateral third and the medial two thirds of the inferior orbital edge (Figure 4A). Theneedle is directed to the apex of the orbit (slightly medially and cephalad) and advanced to a depth of 25-35 mm. Two to 4 mL of LA solution is then injected. An additional facial nerve block is performed to prevent blinking; the technique most frequently used is the Van Lindt block (21). FigFigure 4: The classic technique of peribulbar anesthesia involves two injections:
Alternative Techniques
The Atkinson up-and-in position of the gaze was abandoned when Liu and colleagues (22) and Unsold and colleagues (23) warned that it increases the risk of optic nerve injury. Indeed, this position places the optic nerve near the path of the needle. Moreover, the optic nerve is stretched and can be injured easily by the needle rather than being pushed aside. Alternative puncture sites and specially designed bent or curved needles have been proposed but have never gained popularity.(24–26) RBA is used less frequently today, at least in part because of its risks of complications. Peribulbar Anesthesia With peribulbar anesthesia, the needle is introduced into the extraconal space.(18,19,27,28) The injected volume of LA (6–12 mL) is larger than that for a retrobulbar injection. This larger volume allows the LA to spread into the whole corpus adiposum of the orbit, including the intraconal space, where the nerves to be blocked are located. Additionally, such a large volume allows anterior spread of LA to the lids to provide a block of the orbicularis muscle and to avoid the need for additional lid block. The classic technique involves two injections. The first injection is inferior and temporal, the needle being introduced at the same site as for an RBA injection, but with a smaller up-and-in angle. The second injection is superior and nasal between the medial third and the lateral two thirds of the orbital roof edge (Figure 4B). Alternative Techniques Several alternative techniques of peribulbar anesthesia have been described (Figure 5). The most common sites for needle insertion are (1) medial canthus peribulbar anesthesia,29 (2) lacrimal caruncle,30,31 and (3) inferior and temporal peribulbar injections.(18,19)
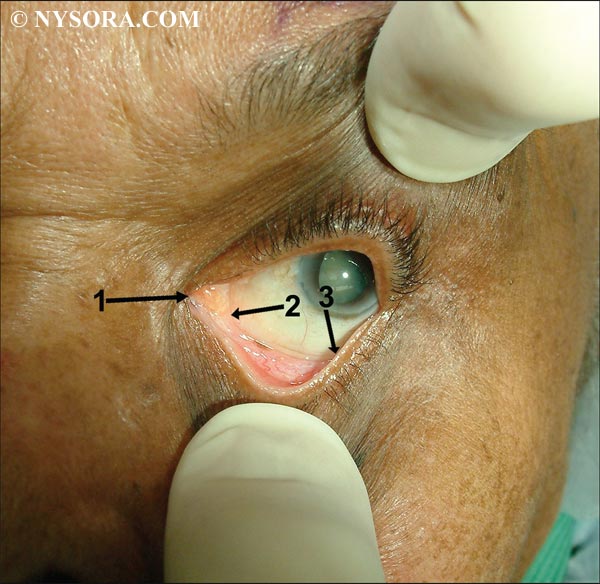
Figure 5: Site of introduction of the needle for the most frequently used blocks: (1) medial canthus peribulbar Retrobulbar Versus Peribulbar Blocks Retrobulbar block has been traditionally assumed to bemore effective than PBA. However, when a sufficient volume of LA is injected, both blocks have similar success rates.38 There is a sound anatomic explanation for this: the absence of an intermuscular membrane to separate extra- from intraconal compartments results in a similar space for the spread of local anesthetic.(14–17) Therefore, if the effectiveness is similar, one would prefer to use the technique with less risk of complications. Because the retrobulbar block theoretically carries a higher risk of complications (optic nerve injury, brainstem anesthesia, retrobulbar hemorrhage), peribulbar block is deemed preferable to retrobulbar block. Major Complications of Eye Blocks The primary cause of serious complications is needle misplacement. Although some anatomic features may increase the risk of complications, the main risk factor is inadequate knowledge and limited experience on the part of the physician. However, it should be noted that complications such as retrobulbar hemorrhage may occur with even the most experienced practitioners. Presenting signs, symptoms, and mechanism of common complications are summarized in Tables 1 and 2.
Central nervous system complications of eye blocks may occur following a needle block by two different mechanisms: An unintentional intraarterial injection may reverse the blood flow in the ophthalmic artery up to the anterior cerebral or the internal carotid artery, (40) so that an injected volume as small as 4 mL may produce seizures. Symptomatic treatment by maintaining patent airway; providing oxygenation; and abolishing seizure activity with small doses of benzodiazepam, propofol, or barbiturates, is usually adequate and results in a rapid recovery without sequelae. An unintentional injection under the dura mater sheath of the optic nerve or directly through the optic foramenmay result in subarachnoid spread of the LA.This causes partial or total brainstem anesthesia. (41–43) Katsev and coworkers (36) have shown that the apex of the orbit may be reached with a 40-mm needle in up to 11% of patients. (36) Depending on the dose and volume of LA spreading toward the brainstem, a bilateral block; cranial nerve palsy with sympathetic activation, confusion, and restlessness; or total spinal anesthesia with tetra paresis, arterial hypotension, bradycardia, and eventually respiratory arrest can occur. Symptomatic treatment (oxygen, vasopressors, and, if required, tracheal intubation and ventilation) should permit complete recovery after the spinal block wears off (a few hours). Unintentional globe perforation and rupture is the most devastating complication of eye blocks. It has a poor prognosis, especially when the diagnosis is delayed. The incidence is between 1 in 350 and 7 in 50,000 cases. (44,45) Main risk factors include inadequate experience of the physician and a highly myopic eye (i.e., long eyeball).(46) In a study of 50,000 cases, Edge and Navon (45) observed thatmyopic staphyloma was a significant risk factor. This suggests that isolated high myopia may not be a risk factor per se but acts as a confounding factor because myopic staphyloma occurs only in myopic eyes.(45) Vohra and Good (46) have observed with B-mode ultrasound that the probability of staphyloma is greater in highly myopic than in slightly myopic eyes. Moreover, staphyloma was more frequently located at the posterior pole of the globe (accounting for perforations after RBA) or in the inferior area of the globe (accounting for perforations after inferior and temporal punctures, both peri- and retrobulbar). As a result, at least in myopic patients and at best in all patients, ultrasound measurement of the axial length of the globe (biometry) should be available. In cases of high myopic eye (axial length greater than 26 mm), a needle block can carry an increased risk of globe perforation. In these cases, a sub-Tenon's or topical block may be preferable. Injury to an extraocular muscle may cause diplopia and ptosis. Several mechanisms can be involved, including direct injury by the needle resulting in intramuscular hematoma, high pressure because of injection into the muscle sheath, or myotoxicity of the LA.(47) The injury may progress in three steps: first, the muscle is paralyzed; second, it seems to recover; and third, a retractile scar develops.
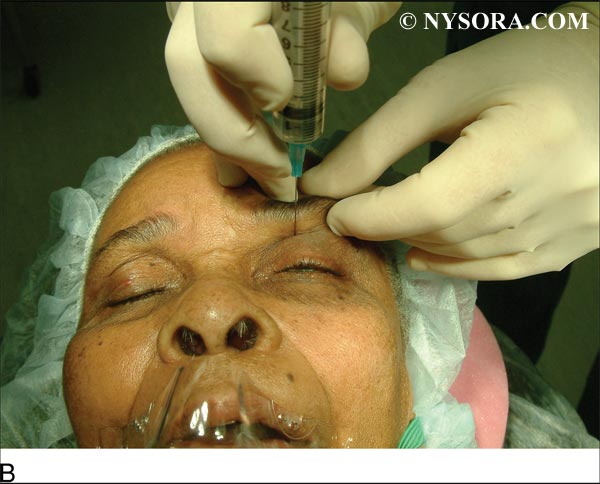
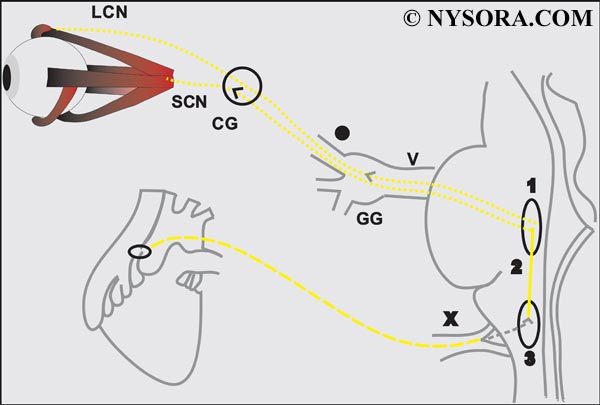 Figure 6: Oculocardiac reflex pathways. LCN = long ciliary nerve; SCN = short ciliary nerve; CG = ciliary ganglion; GG = geniculate ganglion; V = fifth cranial nerve; X = tenth cranial nerve; (1) main sensory nucleus of the trigeminal nerve; (2) short internuncial fibers in the reticular formation (3) motor nucleus of the vagus nerve. Direct optic nerve trauma by the needle is rare but causes blindness. Computed tomography imaging usually shows optic nerve enlargement caused by intraneural hematoma.(35,49) Overall, there is a 1–3% chance of complications, often necessitating postponement of the planned surgery. Since some complicationsmay be life-threatening if patients are not immediately resuscitated, it is recommended that an anesthesiologist be present and monitor the patient perioperatively.(50) Topical Anesthesia 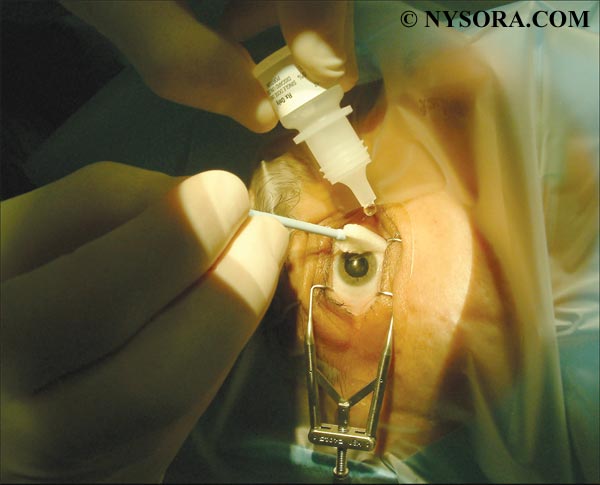 Figure 7: Application of topical anesthesia to the eye. Instillation of LA eye drops provides corneal anesthesia, thus allowing cataract surgery by phacoemulsification (Figure 7). It is quick and simple to perform and avoids the potential hazards of needle techniques. The technique is used in up to 50% of the cataract surgeries performed worldwide. Some surgeons prefer topical anesthesia for routine phacoemulsification in more than 90% of their cases; however, its effectiveness is limited. The lack of akinesia and intraocular pressure control, associated with its short duration, may make surgery hazardous.(51) Therefore, use of topical anesthesia should be limited to uncomplicated procedures performed by experienced surgeons in cooperative patients. Whenever phacoemulsification is not possible, total akinesia is still required and topical anesthesia is questionable. This may be the case inworld areas in which phacoemulsification is not technically available and in some specific indications.(52,53) Because anesthesia may be incomplete, patients randomly subjected to one of these techniques for one eye and the other technique for the other eye prefer the retrobulbar to the topical technique (71% vs 10%).(54) Intraoperative comfort is more constantly obtained under retrobulbar (51,54) or sub-Tenon's (55) than under topical anesthesia. Topical anesthesia appears to be no more effective than no anesthesia in selected cases for an experienced surgeon.(56) Intracameral injection of LA has been proposed to enhance analgesia.(57) It consists of injecting small LA amounts (0.1 mL) in the anterior chamber at the beginning of, or during, surgery. Intracameral anesthetic needs to be preservative-free. Some concerns have been expressed about the toxicity effects of LA on corneal endothelium, which is unable to regenerate. The safety of intracameral injection seems acceptable in this regard,(58)] but its analgesic benefit when compared with simple topical anesthesia has not been established.(56,59-61) This is not surprising because analgesia is not correlated with intracameral LA concentration.(62) The insertion of sponges soaked in LA into the conjunctival fornices has been proposed.(63) The use of lidocaine jelly instead of eye drops seems to enhance the quality of analgesia of the anterior segment (55,62,64) and is becoming very popular for improving the patient's comfort under topical anesthesia. Perilimbar (subconjuctival) Anesthesia Subconjunctival injection of LA may provide analgesia of the anterior segment without akinesia. This technique is not popular. Episcleral (sub-tenon's) blocks Common Principle Episcleral (sub-Tenon's) anesthesia, sometimes also called parabulbar anesthesia, places the injection into the episcleral space. This allows the LA to spread circularly around the scleral portion of the globe, ensuring high-quality analgesia of the whole globe with relatively low injected volumes (usually 3-5 mL).(65,66) In addition, use of a larger volume (up to 8-11 mL) causes the LA to spread to the extraocular muscle sheaths, ensuring effective and reproducible akinesia.(65-68) The occurrence of a chemosis (subconjunctival spread of the LA) is almost mandatory after injecting such large volumes. It confirms the sub-Tenon's location of the injection and requires compression to resolve itself. Several approaches have been described, including needle and no-needle surgical approaches. 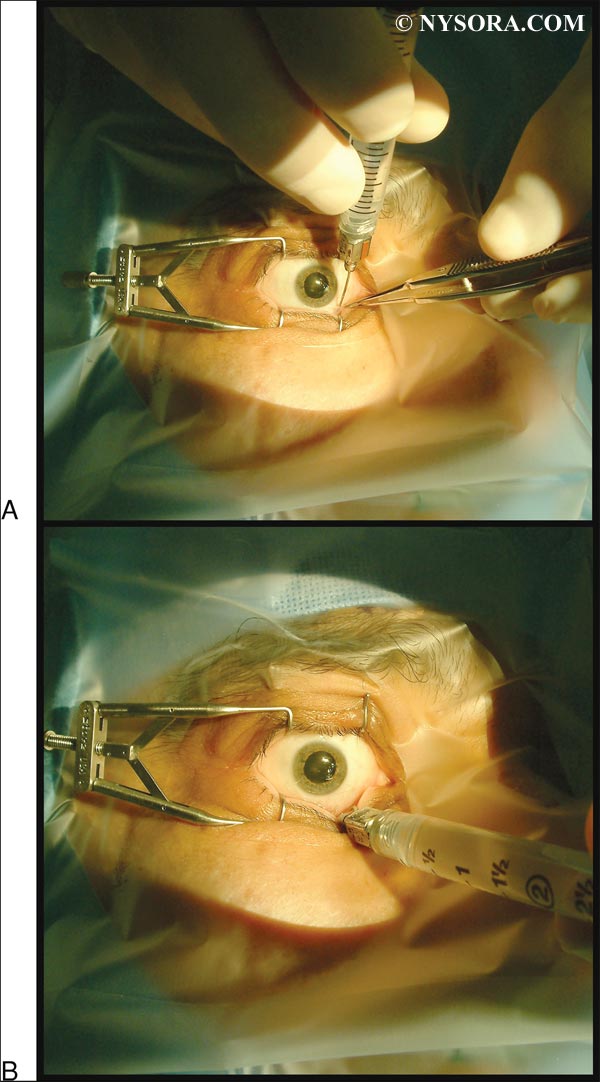 Figure 8: Sub-Tenon's (episcleral) block: The needle is introduced into the fornix between the semilunaris fold of the conjunctiva and the globe, tangentially to the globe. Needle Technique The needle is introduced into the fornix between the semilunaris fold of the conjunctiva and the globe, tangentially to the globe (Figure 8).(65-67,69) After it has encroached the conjunctiva, the needle is slightly shifted medially and advanced strictly posteriorly, therefore attracting the globe and directing the gaze medially. After a small loss of resistance (click) is perceived, the globe comes back to its primary gaze position. This serves as a depth marker, thus indicating injection depth at 10 to 15 mm. The volume injected may be up to 10 mL, depending on the patient's anatomy. Using a large volume with this technique (6-11 mL) results in good globe and eye lid akinesia that is more reproducible than classic peribulbar anesthesia.(67) This technique is associated with a low risk of complications and it is simple to learn and use. In a series of 2000 cases no serious complications occurred.(69) However, as for all needle techniques, the risk of misplacement of the needle and its subsequent complications must be always kept in mind. Surgical Approach This technique was first proposed as a supplement to (or rescue block) RBA.(70,71) After topical anesthesia, the bulbar conjunctiva is grasped with a small forceps in the inferior and nasal, superior and nasal, or superior and temporal quadrant, 5-10 mm from the limbus. Small scissors are used to open a small opening into the conjunctiva and Tenon's capsule to gain access to the episcleral space. A blunt cannula is then inserted into the episcleral space to allow the injection.(72,73) When a specialized cannula is not available, a short intravenous catheter (18- or 20-gauge) can also be used. This technique is typically used with injection of low volumes of LA (3-5 mL). It provides good globe analgesia but only partial akinesia of the globe and lids.74 The injection causes only a minor increase in intraocular pressure, so that preoperative compression of the globe is typically unnecessary. In a similar way, episcleral injection of a small volume of LA may be used on an open globe; it is the technique of choice as an intraoperative supplemental injection when anesthetic technique appears insufficient during surgery. Increasing the injected volume (e.g., Use of Eye Block For Postoperative Analgesia All available LAs have been used for eye block, either alone or as a mixture of two different agents. The LA's used most oftenare lidocaine, bupivacaine, ropivacaine, mepivacaine, or a combination of two of these. The choice of LAs should be based on the pharmacologic properties and availability of the drugs, mainly depending on the requirement for a quick onset (lidocaine, mepivacaine), prolonged effect or postoperative residual block for analgesia (ropivacaine, bupivacaine), or akinesia (higher concentration). Because the amount of LA injected is usually small (3-11 mL), systemic toxicity is not a major concern. Hyaluronidase is an enzyme that has been proposed to hasten the onset and increase the success rate of regional anesthesia for the eye. However, the literature is somewhat controversial about its real benefit concerning akinesia.(77,78) Another possible benefit of hyaluronidase is in the lesser incidence of postoperative strabismus connected with its use, possibly by limiting LA myotoxicity owing to its faster spread.(79,80) Clonidine enhances intra- and postoperative analgesia when added to the LA. At a dose of 1 mcg/kg, it does not increase the incidence of systemic adverse events such as hypotension or excessive sedation.(81) Moreover, it may help to prevent intraoperative arterial hypertension and lower intraocular pressure. Epinephrine is sometimes used to increase the duration of eye block. However, the availability of long-acting LAs has decreased its value. Fear of vasospasm and subsequent retinal ischemia is probably not justified because the LA mixture does not spread inside the globe where retinal arteries are located. Alkalinization of local anesthetic solutions has been proposed for decreasing pain during injection and accelerating the block onset; however, its efficacy remains unproven. Other adjuvant agents have been proposed but have not gained popularity. Small doses of a muscle relaxant may enhance akinesia, but concern has been expressed about their potential risk for systemic effects.(82) Opioids do not appear to be more efficient via a regional ophthalmic route than via systemic administration.(83) Warming the LA may decrease pain on injection and enhance block efficacy, but its benefit appears clinically irrelevant.(84) Who Should Perform Eye Blocks Since the 1980s, anesthesiologists have become increasingly involved in eye blocks that previously were performed by surgeons. However, in some countries, anesthesiologists are not available, and surgeons have to manage the block themselves.(85) In other countries, anesthesiologists only monitor the anesthesia care, as the surgeon performs the block. On the other hand, anesthesiologists are often responsible for administering regional anesthesia in France and the United Kingdom. The available literature suggests that with proper training, anesthesiologists can perform eye blocks with the same degree of safety as for other regional anesthesia techniques.(24,29,69,74) Perioperative Management Eye surgery (e.g., cataract surgery) carries a low risk of perioperative morbidity and mortality.(86–88) Eye block is associated with lower perioperative morbidity than is general anesthesia used for ophthalmic surgery, provided that heavy sedation is avoided.(87,88) Intraoperative monitoring should include basic monitoring (ie, electrocardiogram, pulse oximetry, and automated noninvasive blood pressure measurement). An intravascular access is required. Older patients undergoing eye surgery frequently have coexisting diseases such as diabetes mellitus, hypertension, coronary artery disease, or cardiac insufficiency. A preoperative assessment should be routinely done to ensure that coexisting medical conditions are reasonably well controlled. Anxiety and residual pain frequently occur during eye surgery under LA. Perfect immobility is required, and the presence of drapes over the head increases anxiety and impairs access to the airway. The patient should be positioned as comfortably as possible, with sufficient space to allow free breathing. Intraoperative sedation with judicious doses of sedatives may be used to limit anxiety and pain. However, an excess of sedation may lead to restlessness, sleeping, snoring, or respiratory depression, which, in the absence of any airway access, pose a significant intraoperative challenge. Maintenance of meaningful patient contact is of paramount importance to avoid disasters that can occur with disoriented or combative patients while the surgery is underway. Summary In summary, in developed countries, eye surgery is among the most frequently performed surgical procedures requiring anesthesia.During the past 20 years, anesthesiologists have assumed a growing role in performing eye blocks. The requirement for a deep anesthetic block with total akinesia has been greatly lessened by use of phacoemulsification for cataract surgery, giving a more prominent role to topical anesthesia. Needle blocks carry a low but real risk of serious complications, mainly because of needle misplacement. Training and practice are required to prevent such problems. The major patient risk factor is the presence of a myopic staphyloma. A surgical approach, sub-Tenon's block, lessens the risks of needle blocks but does not completely prevent complications. When akinesiaanda dense block are required, the sub-Tenon's block appears to be the technique of choice. REFERENCES: 1. Leaming DV: Practice styles and preferences of ASCRS members- 2003 survey. J Cataract Refract Surg 2004;30:892-900. 2. QuigleyHA:Mortality associatedwith ophthalmic surgery:A20-year experience at the Wilmer Institute. Am J Ophthalmol 1974;77:517-524. 3. Breslin PP: Mortality in ophthalmic surgery. Int Ophthalmol Clin 1973;13:215-226. 4. McKibbinM:Thepre-operative assessment and investigationofophthalmic patients. Eye 1996;10:138-140. 5. Bass EB, Steinberg EP, Luthra R: Do ophthalmologists, anesthesiologists, and internists agree about preoperative testing in healthy patients undergoing cataract surgery? Arch Ophthalmol 1995;113:1248-1256. 6. Maltzman BA, Cinotti AA, Calderone JP Jr: Preadmission evaluation and elective cataract surgery. J Med Soc N J 1981;78:519-520. 7. Gilvarry A, Eustace P: Themedical profile of cataract patients. Trans Ophthalmol Soc U K 1982;102:502-504. 8. Fisher SJ, Cunningham RD: Themedical profile of cataract patients. Clin Geriatr Med 1985;1:339-344. 9. Hardesty DC: The Ophthalmic Surgical Patient, Medical Perioperative Management. Edited by Wolfsthal S. Appleton & Lange, 1989, pp 417-426 10. Gild WM, Posner KL, Caplan RA, et al: Eye injuries associated with anesthesia. A closed claims analysis. Anesthesiology 1992;76:204-208 11. Hodgkins P, Luff A,MorrellA:Current practice of cataract extraction and anaesthesia. Br J Ophthalmol 1992;76:323-326. 12. Hamilton R, Gimble H, Strunin L: Regional anaesthesia for 12,000 cataract extraction and intraocular lens implantation procedures. JCan Anaesth 1988;35:615-623. 13. Eke T, Thompson J: The national survey of local anaesthesia for ocular surgery. II. Survey methodology and current practice. Eye 1999;13:196-204. 14. Ropo A,Nikki P, Ruusuvaara P, et al: Comparison of retrobulbar and periocular injections of lignocaine by computerized tomography. Br J Ophthalmol 1991;75:417-420. 15. Koornneef L: The architecture of the musculo-fibrous apparatus in the human orbit. Acta Morphol Neerl Scand 1977;15:35-64. 16. Koornneef L: Details of the orbital connective tissue system in the adult. Acta Morphol Neerl Scand 1977;15:1-34. 17. Ripart J, Lefrant J, de La Coussaye J, et al: Peribulbar versus retrobulbar anesthesia for ophthalmic surgery. An anatomical comparison of extraconal and intraconal injections. Anesthesiology 2001;94:56-62. 18. Bloomberg L: Administration of periocular anesthesia. J Cataract Refract Surg 1986;12:677-679. 19. Davis D, Mandel M: Posterior peribulbar anesthesia: An alternative to retrobulbar anesthesia. J Cataract Refract Surg 1986;12:182-184. 20. AtkinsonW: Retrobulbar injection of anestheticwithin themuscular cone (cone injection). Arch Ophthalmol 1936;16:495-503. 21. Liu C, Youl B, Moseley I: Magnetic resonance imaging of the optic nerve in the extremes of gaze. Implications for the positioning of the globe for retrobulbar anaesthesia.Br JOphthalmol 1992;76:728-733. 22. Van Lindt M: Paralysie palpébrale transitoire provoquée dans l'operation de la cataracte. Ann Ocul 1914;151:420-424. 23. Unsöld R, Stanley J, Degroot J: The C.T. topography of retrobulbar anesthesia. Anatomical correlation of implications and suggestion of a modified technique Albrecht Von Graefes. Arch Klin ExpOphthalmol 1981;217:125-136. 24. Hamilton R, Loken R: Modified retrobulbar block. Can J Anaesth 1993;40:1219-1220. 25. Galindo A, Keilson L, Mondshine R, et al: Retro-peribulbar anesthesia: Special technique and needle design. Ophthalmol Clin North Am 1990;3:71-81. 26. Straus J: A new retrobulbar needle injection technique. Ophthalmic Surg 1988;19:134-139. 27. Bloomberg L: Anterior periocular anaesthesia: Five years experience. J Cataract Refract Surg 1991;17:508-511. 28. Davis D,Mandel M: Efficacy and complication rate of 16224 consecutive peribulbar blocks. A prospective multicenter study. J Cataract Refract Surg 1994;20:327-337. 29. Hustead R,Hamilton R, Loken R: Periocular local anesthesia: Medial orbital as an alternative to superior nasal injection. J Cataract Refract Surg 1994;20:197-201. 30. Wang BC, Bogart B, Hillman DE, et al: Subarachnoid injection— A potential complication of retrobulbar block. Anesthesiology 1989;71:845-857. 31. Kumar CM, Lawler PG: Pulmonary oedema after peribulbar block. Br J Anaesth 1999;82:777-779. 32. Demirok A, Simsek S,Cinal A, et al:Peribulbar anesthesia:Oneversus two injections Ophthalmic Surg Lasers 1997;28:998-1001. 33. Ball JL,WoonWH,Smith S: Globe perforation by the second peribulbar injection. Eye 2002;16:663-665. 34. Sarvela J,Nikki P:Comparison of two needle lengths in regional ophthalmic anesthesia with etidocaine and hyaluronidase. Ophthalmic Surg 1992;23:742-745. 35. Karampatakis V, Natsis K, Gisgis P, Stangos N: The risk of optic nerve injury in retrobulbar anesthesia: A comparative study on 35 and 40 mm retrobulbar needles in 12 cadavers. Eur J Ophthalmol 1998;8:184-187. 36. Katsev D, Drews RC, Rose BT: Anatomic study of retrobulbar needle path length. Ophthalmology 1989;96:1221-1224. 37. Waller S, Taboada J, O'Connor P: Retrobulbar anesthesia risk: Do sharp needles really perforate the eyemore easily than blunt needles? Ophthalmology 1993;100:506-510. 38. DemediukO, Dhaliwal R,PapworthD, et al:Acomparisonofperibulbar and retrobulbar anesthesia for vitreoretinal surgical procedures. Arch Ophthalmol 1995;113:908-913. 39. Rainin EA, Carlson BM: Postoperative diplopia and ptosis. A clinical hypothesis based on the myotoxicity of local anesthetics. Arch Ophthalmol 1985;103:1337-1339. 40. Aldrete J, Romo-Salas F, Arora S, et al: Reverse arterial blood flow as a pathway for central nervous system toxic responses following injection of local anesthetics. Anesth Analg 1978;57:428-433. 41. Singer SB, Preston R, Hodge WG: Respiratory arrest following peribulbar anesthesia for cataract surgery: Case report and review of literature. Can J Ophthalmol 1997;32:450-454. 42. Loken R, Mervyn Kirker GE, Hamilton RC: Respiratory arrest following peribulbar anesthesia for cataract surgery: Case report and review of the literature. Can J Ophthalmol 1998;33:225-226. 43. Nicoll J, Acharya P, Ahlen K, et al: Central nervous system complication after 6000 retrobulbar blocks. Anesth Analg 1987;66:1298-1302. 44. Duker J, Belmont J, Benson W, et al: Inadvertent globe perforation during retrobulbar and peribulbar anesthesia. Ophthalmology 1991;98:519-526. 45. Edge R,Navon S: Scleral perforation during retrobulbar and peribulbar anesthesia: Risk factor and outcome in 50,000 consecutive injections. J Cataract Refract Surg 1999;25:1237-1244. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
![[advertisement] gehealthcare](../../files/banners/banner1_250x600/GEtouch(250X600).gif)







 Educational Material Download
Educational Material Download








Post your comment