Ankle Block
|
Figure 1: Needle insertion for saphenous nerve block of the ankle. Essentials
General Considerations An ankle block is essentially a block of four terminal branches of the sciatic nerve (deep and superficial peroneal, tibial, and sural) and one cutaneous branch of the femoral nerve (saphenous). Ankle block is simple to perform, essentially devoid of systemic complications, and highly effective for a wide variety of procedures on the foot and toes. For this reason, this technique should be in the arma mentarium of every anesthesiologist. At our institution, an ankle block is most commonly used in podiatric surgery and foot and toe debridement or amputation. Functional Anatomy It is useful to think of the ankle block as a block of two deep nerves (posterior tibial and deep peroneal) and three superficial nerves (saphenous, sural, and superficial peroneal). This concept is important for success of the block because the two deep nerves are anesthetized by injecting local anesthetic under the fascia, whereas the three superficial nerves are anesthetized by a simple subcutaneous injection of local anesthetic. Common Peroneal Nerve The common peroneal nerve separates from the tibial nerve and descends alongside the tendon of the biceps femoris muscle and around the neck of the fibula. Just below the head of the fibula, the common peroneal nerve divides into its terminal branches: the deep peroneal and superficial peroneal nerves. The peroneus longus muscle covers both nerves. Deep Peroneal Nerve The deep peroneal nerve runs downward below the layers of the peroneus longus, extensor digitorum longus, and extensor hallucis longus muscles to the front of the leg (Figure 2). At the ankle level, the nerve lies anterior to the tibia and the interosseous membrane and close to the anterior tibial artery. It is usually sandwiched between the tendons of the anterior tibial and extensor digitorum longus muscles. At this point, it divides into two terminal branches for the foot: the medial and the lateral. The medial branch passes over the dorsum of the foot, along the medial side of the dorsalis pedis artery, to the first interosseous space, where it supplies the web space between the first and second toe. The lateral branch of the deep peroneal nerve is directed anterolaterally, penetrates and innervates the extensor digitorum brevis muscle, and terminates as the second, third, and fourth dorsal interosseous nerves. These branches provide innervation to the tarsometatarsal, metatarsophalangeal, and interphalangeal joints of the lesser toes. Superficial Peroneal Nerve The superficial peroneal nerve (also called the musculocutaneous nerve of the leg) provides muscular branches to the peroneus longus and brevis muscles. After piercing the deep fascia covering the muscles, the nerve eventually emerges from the anterolateral compartment of the lower part of the leg and surfaces from beneath the fascia 5 to 10 cm above the lateral malleolus (Figure 3). At this point, it divides into terminal cutaneous branches: the medial and the lateral dorsal cutaneous nerves (Figure 4A and B). These branches carry sensory innervation to the dorsum of the foot and communicate with the saphenous nerve medially, as well as the deep peroneal nerve in the first web space and the sural nerve on the lateral aspect of the foot.
Figure 2: Anatomy of the ankle. (1) artery dorsal pedis, (2) deep peroneal nerve.
Figure 3: Anatomy of the ankle. (1) superficial peroneal nerve. (2) sural nerve. Tibial Nerve The tibial nerve separates from the common popliteal nerve proximal to the popliteal fossa crease and joins the tibial artery behind the knee joint. The nerve runs distally in the thick neurovascular fascia and emerges at the inferior third of the leg from beneath the soleus and gastrocnemius muscles on the medial border of the Achilles tendon (Figure 5). At the level of the medial malleolus, the tibial nerve is covered by the superficial and deep fasciae of the leg. It is positioned laterally and posteriorly to the posterior tibial artery and midway between the posterior aspect of the medial malleolus and the posterior aspect of the Achilles tendon. Just beneath the malleolus, the nerve divides into lateral and medial plantar nerves. The posterior tibial nerve provides cutaneous, articular, and vascular branches to the ankle joint, medial malleolus, inner aspect of the heel, and Achilles tendon. It also branches to the skin, subcutaneous tissue, muscles, and bones of the sole. Sural Nerve The sural nerve is a sensory nerve formed by a union of the medial sural nerve (a branch of the tibial nerve) and the lateral sural nerve (a branch of the common peroneal nerve). The sural nerve courses between the heads of the gastrocnemius muscle, and after piercing the fascia covering the muscles, it emerges on the lateral aspect of the Achilles tendon 10 to 15 cm above the lateral malleolus (Figure 4A and B). After providing lateral calcaneal branches to the heel, the sural nerve descends behind the lateral malleolus, supplying the lateral malleolus, Achilles tendon, and ankle joint. The sural nerve continues on the lateral aspect of the foot, innervating the skin, subcutaneous tissue, fourth interosseous space, and fifth toe.
Figure 4: (A) Anatomy of the ankle. (1) Sural nerve. (2),(3) Superficial peroneal nerve. (B) Anatomy of the ankle. (1) Sural nerve, (2) Superficial peroneal nerve.
Saphenous Nerve The saphenous nerve is a terminal cutaneous branch (or branches) of the femoral nerve. Its course is in the subcutaneous tissue of the skin on the medial aspect of the ankle and foot (Figure 6).
Distribution of Blockade An ankle block results in anesthesia of the foot. However, note that an ankle block does not result in anesthesia of the ankle itself. The proximal extension of the blockade is to the level at which the block is performed. The more proximal branches of the tibial and peroneal nerves innervate the deep structures of the ankle joint. The two deep nerves (tibial and deep peroneal) provide innervation to the deep structures, bones, and cutaneous coverage of the sole and web between the first and second toes (Figure 7). Equipment A standard regional anesthesia tray is prepared with the following equipment:
Landmarks and Patient Positioning The patient is in the supine position with the foot on a footrest.
Figure 7: Innervation of the foot.
Figure 8: (A) Maneuvers to extenuate the extensor tendons. The deep peroneal nerve is located lateral to the hallucis longus tendon (line). (B) Deep peroneal block. The needle is inserted just lateral to the hallucis longus tendon and slowly advanced to contact the bone. Upon bone contact, the needle is withdrawn 2-3 mm, and 5 mL of local anesthetic is injected. The deep peroneal nerve is located immediately lateral to the tendon of the extensor hallucis longus muscle (between the extensor hallucis longus and the extensor digitorum longus) (Figure 8). The pulse of the anterior tibial artery (dorsalis pedis) can be felt at this location; the nerve is positioned immediately lateral to the artery. The posterior tibial nerve is located just behind and distal to the medial malleolus. The pulse of the posterior tibial artery can be felt at this location; the nerve is just posterior to the artery. The superficial peroneal, sural, and saphenous nerves are located in the subcutaneous tissue along a circular line stretching from the lateral aspect of the Achilles tendon across the lateral malleolus, anterior aspect of the foot, and medial malleolus to the medial aspect of the Achilles tendon.
Technique For time-efficient blockade of all five nerves, the operator should walk from one side of the foot to the other during the block procedure instead of bending and leaning over to reach the opposite side. Before beginning the procedure, the entire foot should be cleaned with a disinfectant. It makes sense to begin this procedure with blocks of the two deep nerves because subcutaneous injections for the superficial blocks often deform the anatomy. A controlled or regular syringe can be used. Deep Peroneal Nerve Block The finger of the palpating hand is positioned in the groove just lateral to the extensor hallucis longus (Figure 8A). The needle is inserted under the skin and advanced until stopped by the bone. At this point, the needle is withdrawn back 1 to 2 mm, and 2 to 3 mL of local anesthetic is injected (Figure 8B).
Figure 9: (A) Landmark for posterior tibial nerve block is found by palpating the pulse of the tibial artery posterior to the medial malleolus. (B) Posterior tibial nerve block is accomplished by inserting the needle next to the pulse of the tibial artery. The needle is advanced until contact with the bone is established. At this point the needle is withdrawn 2-3 mm, and 5 mL of local anesthetic is injected. Posterior Tibial Nerve Block The posterior tibial nerve is anesthetized by injecting local anesthetic just behind the medial malleolus (Figure 9A). Similar to that of the deep peroneal nerve, its position is deep to the superficial fascia. The needle is introduced in the groove behind the medial malleolus and advanced until contact with the bone is felt. At this point, the needle is with- drawn back 1 to 2 mm, and 2 to 3 mL of local anesthetic is injected (Figure 9B).
Blocks of the Superficial Peroneal, Sural, and Saphenous Nerves  Figure 10: Saphenous nerve block is accomplished by injection of local anesthetic in a circular fashion (line) subcutaneously just above the medial malleolus. These three nerves are superficial cutaneous extensions of the sciatic and femoral nerves. Because they are positioned superficially to the deep fascia, an injection of local anesthetic in the territory through which they descend to the distal foot is adequate to achieve their blockade. Each nerve is blocked using a simple circumferential injection of local anesthetic subcutaneously (Figures 10, 11, and 12). To block the saphenous nerve, a 1.5 in, 25-gauge needle is inserted at the level of the medial malleolus and a "ring" of local anesthetic is raised from the point of needle entry to the Achilles tendon and anteriorly to the tibial ridge (Figure 10). This can be usually accomplished with one or two needle insertions; 5 mL of local anesthetic suffices. To block the superficial peroneal nerve, the needle is inserted at the tibial ridge and extended laterally toward the lateral malleolus (Figure 11). It is important to raise a subcutaneous "wheal" during injection, which indicates injection in the proper superficial plane. Five milliliters of local anesthetic is adequate. To block the sural nerve, the needle is inserted at the level of the lateral malleolus and the local anesthetic is infiltrated toward the Achilles tendon (Figure 12). Five milliliters of local anesthetic is deposited in a circular fashion to raise a skin "wheal."
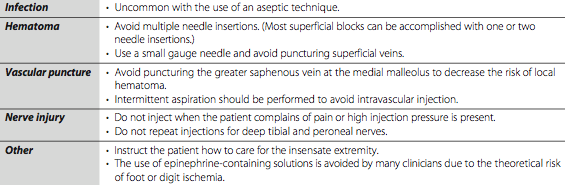
Block Dynamics and perioperative Management Ankle block is one of the more uncomfortable block procedures for patients. The reason is that it involves five separate needle insertions, and subcutaneous injections to block the cutaneous nerves result in discomfort due to the pressure distension of the skin and nerve endings. Additionally, the foot is supplied by an abundance of nerve endings and is exquisitely sensitive to needle injections. For these reasons, this block requires significant premedication to make it acceptable to patients. We routinely use a combination of midazolam (2-4 mg intravenously) and a narcotic (500-750 µg alfentanil) to ensure the patient's comfort during the procedure. A typical onset time for this block is 10 to 25 minutes, depending primarily on the concentration and volume of local anesthetic used. Placement of an Esmarch bandage or a tourniquet at the level of the ankle is well-tolerated and typically does not require additional blockade in sedated patients. Complications and How to Avoid Them Complications following an ankle block are typically limited to residual paresthesias due to inadvertent intraneuronal injection. Systemic toxicity is uncommon because of the distal location of the blockade. Table 1 provides more specific instructions on possible complications and corrective measures. Table 1: Complications of Ankle Block and Preventive Techniques
|
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)






























Post your comment