Axillary Brachial Plexus Block
Figure 1: The needle is inserted toward the axillary artery (line) until either motor response of the hand or arterial blood on aspiration is obtained. Essentials
General Considerations The axillary brachial plexus block was first described by Halsted in 1884 at the Roosevelt Hospital in New York City. The axillary brachial plexus block is one of the most commonly used regional anesthesia techniques. The proximity of the terminal nerves of the brachial plexus to the axillary artery makes identification of the landmarks consistent (axillary artery) equally for both the nerve stimulator and surface based ultrasound-guided techniques. The axillary block is an excellent choice of anesthesia technique for elbow, forearm, and hand surgery. Functional Anatomy By the time the brachial plexus passes behind the lower bor- der of the pectoralis minor muscle in the axilla, the cords quickly begin to form the principal terminal nerves of the brachial plexus, namely, the median, ulnar, radial, and musculocutaneous nerves (Figure 2). The arrangement of the individual nerves and their relationship to the axillary artery is important in axillary blockade (Figure 3). With the arm abducted at 90° and the axillary arterial pulsation as a point of reference, the nerves are located as follows: The median nerve is positioned superficially and immediately above the pulse; the ulnar nerve is found superficial slightly deeper than the median nerve; the radial nerve is located behind the pulse. The musculocutaneous nerve can be found 1 to 3 cm deeper and above the pulse, often outside the brachial plexus sheath as it moves distally away from the axillary fossa. 
Figure 2: Anatomy of the brachial plexus in the axilla. (1) axillary artery. (2) median nerve. (3) ulnar nerve. (4) radial nerve. (5) musculocutaneous nerve as it enters the cora- cobrachialis muscle. (6) coracoid brachialis muscle. Pectoralis muscles are show retracted laterally (right upper corner). Musculocutaneous Nerve The musculocutaneous nerve is a terminal branch of the lat- eral cord. It pierces the coracobrachialis muscle to descend between the biceps and brachialis muscles, giving innervation to both. The nerve continues distally as the lateral cutaneous nerve of the forearm, which emerges from the deep fascia between the biceps and brachioradialis to emerge superficially at the level of the cubital fossa. From here on, the nerve supplies cutaneous sensory branches to the lateral aspect of the forearm. Median Nerve The median nerve derives its origin from both the lateral and medial cords. It provides motor branches to the flexors of the hand and wrist, and sensation to the palmar surface of the first, second, third digits and the lateral half of the fourth digit. Interestingly, the median and ulnar nerves both traverse the entire length of the arm without giving off branches above the elbow joint. Ulnar Nerve The ulnar nerve is a terminal branch of the medial cord. Together with the medial cutaneous nerve of the forearm, it initially lies medial to the brachial artery but leaves the artery at midarm to pass behind the medial epicondyle to enter the forearm. The ulnar nerve has articular branches to the elbow joint and muscular branches to the hand and forearm. The nerve provides sensory innervation to the fourth and fifth digits. 
Figure 3: Spatial organization of the brachial plexus in the axilla. Note that the musculocutaneous nerve is outside of the axillary plexus sheath. Radial Nerve The radial nerve, a terminal branch of the posterior cord, leaves the axilla by passing below the teres major and between the humerus and the long head of the triceps. The radial nerve supplies branches to the triceps, brachioradialis, and extensor radialis longus muscles. Cutaneous branches innervate the lateral aspect of the arm and the posterior aspect of the forearm and hand. Distribution of Blockade Axillary brachial plexus block provides anesthesia to the elbow, forearm, and hand (Figure 4). Equipment A standard regional anesthesia tray is prepared with the following equipment:
Landmarks and Patient Positioning The patient is placed in the supine position with the head facing away from the side to be blocked. The arm is abducted to form an approximately 90° angle in the elbow joint (Figure 5).
Surface landmarks for the axillary brachial plexus block include the following: 1. Pulse of the axillary artery 2. Coracobrachialis muscle 3. Pectoralis major muscle 
Figure 4: Cutaneous distribution of anesthesia after axillary brachial plexus block. Axillary block results in anesthesia in the labeled areas.
Figure 5:Patient position for the axillary brachial plexus block. Technique After thorough skin preparation, the pulse of the axillary artery is palpated high in the axilla, Figure 6. Once the pulse is felt, the artery is fixed between the index and the middle fingers and firmly pressed against the humerus to prevent "rolling" of the axillary artery during block performance. At this point, movement of the palpating hand and the patient's arm should be minimized because the axillary artery is highly movable in the adipose tissue of the axillary fossa. The anesthesiologist should assume a sitting position by the patient's side to avoid strain and unwanted hand movement during block performance. The index and middle fingers of the palpating hand should be pressed firmly against the arm, straddling the pulse of the axillary artery immediately distal to the insertion of the pectoralis major muscle (Figure 6). This maneuver shortens the distance between the needle insertion site and the brachial plexus block by compressing the subcutaneous tissue. It also helps in stabilizing the position of the artery and needle during performance of the block. The palpating hand should not be moved during the entire procedure to allow for precise redirection of the angle of needle insertion when necessary. Local anesthetic is infiltrated subcutaneously at the determined needle insertion site. Axillary brachial plexus blocks can also be accomplished using multiple injections after electrolocation of each nerve. Several studies have documented faster onset and better success rate compared with the single-injection technique. Multiple injections are possible due to the shallow and relatively predictable location of the nerves. With this technique, the mental image of the position the nerves in relationship to the artery should be kept in mind, Figure 3.
A needle connected to the nerve stimulator (0.5-1.0 mA, 2 Hz, 0.1-0.3 ms) is inserted at an angle of 45° cephalad (Figure 7).

Figure 8: To block the musculocutaneous nerve, the needle is inserted above the axillary artery and directed upward to localize the musculocutaneous nerve. Once through the skin, the needle is slowly advanced directly below the pulse until stimulation of the brachial plexus is obtained. Typically, this occurs at a depth of 1 to 2 cm in most patients. The needle should be advanced gently until a radial nerve twitch (extension of wrist and/or fingers) is obtained, and 10 to 15 mL of local anesthetic is deposited after negative aspiration. The needle is then withdrawn completely and reinserted above the artery without moving the palpating hand (Figure 8). Advancing slowly, the median nerve should be encountered within 1 to 2 cm, resulting in finger flexion. The needle is then advanced slightly deeper until the ulnar twitch reappears. At this point, a further 5 to-10 mL of local anesthetic is deposited after negative aspiration. Finally, through the same insertion site, the needle is brought back to the skin, redirected up into the bulk of the coracobrachialis, and advanced slowly. Once the needle tip is in proximity to the musculocutaneous nerve, the local coracobrachialis twitch will disappear and a more vigorous biceps brachii twitch will materialize. The last 5 to 8 mL of local anesthetic should be administered here. Occasionally, no biceps twitch will be obtained, in which case it is sufficient to deposit the local anesthetic in the substance of the coracobrachialis muscle itself for coverage of the musculocutaneous nerve.
Troubleshooting Some common responses to nerve stimulation and the course of action to obtain the proper response are shown in Table 1. Block Dynamics and Perioperative Management An axillary brachial plexus block is associated with relatively minor patient discomfort at the time of placement. However, some patients complain of the sensation of soreness in the axillary region after the block resolution, which may be related the intramuscular needle insertion or hematoma formation from inadvertent vascular puncture. Intravenous midazolam 1 to 2 mg with alfentanil 250 to 500 µg at the time of needle insertion should produce a comfortable, cooperative patient during nerve localization. The onset time for this block ranges between 15 and 25 minutes. The first sign of the blockade is loss of coordination of the arm and forearm muscles. This sign is usually seen sooner than the onset of a sensory or temperature change. When this sign is observed shortly after injection, it is highly predictive of an oncoming successful brachial plexus blockade. Table 1: Some Common Responses to Nerve Stimulation and the Course of Action for Proper Response 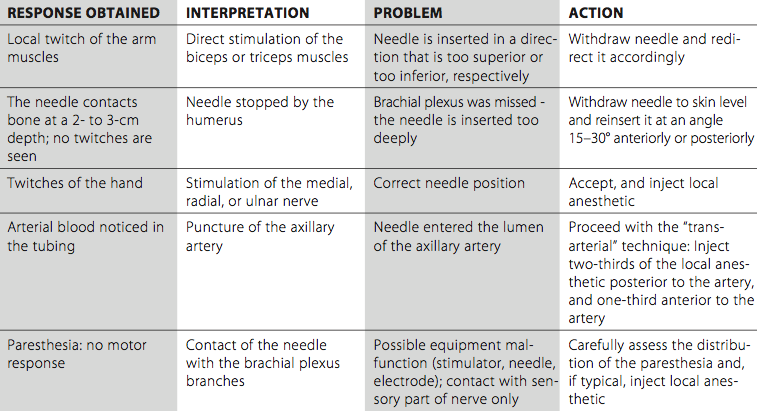
Complications and how to avoid them Table 2: Complications of Axillary Block and Techniques to Avoid them 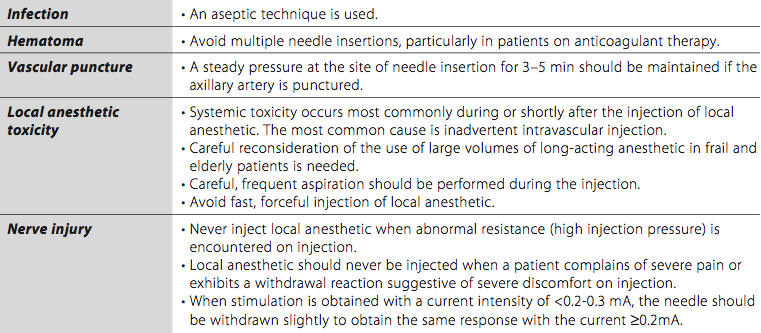 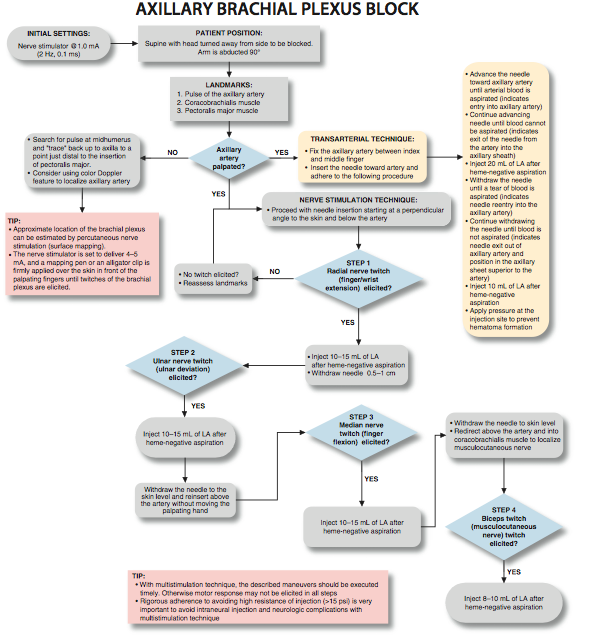    |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)
![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)





















Post your comment