Femoral Nerve Block
|
Figure 1: Needle insertion for femoral nerve block. Essentials
 Figure 2: Anatomy of the femoral triangle. (1) femoral artery. (2) femoral nerve. (3) femoral vein. (4) anterior superior iliac spine. (5) inguinal ligament. (6) sartorius. General Considerations A femoral nerve block is a quintessential nerve block technique that is easy to master, carries a low risk of complications, and has significant clinical application for surgical anesthesia and postoperative pain management. The femoral block is well-suited for surgery on the anterior thigh and knee, quadriceps tendon repair, and postoperative pain management after femur and knee surgery. When combined with a block of the sciatic nerve, anesthesia of almost the entire lower extremity from the midthigh level can be achieved. Functional Anatomy The femoral nerve is the largest branch of the lumbar plexus, arising from the second, third, and fourth lumbar nerves. The nerve descends through the psoas muscle, emerging from the psoas at the lower part of its lateral border, and it runs downward between the psoas and the iliacus. The femoral nerve eventually passes underneath the inguinal ligament into the thigh, where it assumes a more flattened shape (Figure 2). The inguinal ligament is a convergent point of the transversalis fascia (fascial sac lining the deep surface of the anterior abdominal wall) and iliac fascia (fascia covering the posterior abdominal wall). As it passes beneath the inguinal ligament, the nerve is positioned lateral and slightly deeper than the femoral artery between the psoas and iliacus muscles. At the femoral crease, the nerve is on the surface of the iliacus muscle and covered by the fascia iliaca or sandwiched between two layers of fascia iliaca. In contrast, vascular fascia of the femoral artery and vein, a funnel-shaped extension of the transversalis fascia, forms a distinctly different compartment from that of the femoral nerve but often contains the femoral branch of the genitofemoral nerve lateral to the vessels (Figure 3). The physical separation of the femoral nerve from the vascular fascia explains the lack of spread of a "blind paravascular" injection of local anesthetic toward the femoral nerve.
The branches to the sartorius muscle depart from the antero- medial aspect of the femoral nerve toward the sartorius muscle. Because sartorius muscle twitch may be the result of the stimulation of this specific branch and not the femoral nerve, the sartorius motor response should not be accepted. Although the needle in the proper position (close to the main trunk of the femoral nerve) often results in sartorius muscle twitch, quadriceps twitch results in more consistent blockade, and it routinely should be sought before injecting local anesthetic unless ultrasound is used concomitantly. The femoral nerve supplies the muscular branches of the iliacus and pectineus and the muscles of the anterior thigh, except for the tensor fascia lata. The nerve also provides cutaneous branches to the front and medial sides of the thigh, the medial leg and foot (saphenous nerve), and the articular branches of the hip and knee joints (Table 1).
Figure 3: Arrangement of the fascial sheaths at the femoral triangle. Femoral nerve is enveloped by two layers of fascia iliaca, whereas femoral vessels are contained in the vascular (femoral) sheath made up of fascia lata. Distribution of Blockade Table 1: Femoral Nerve Branches 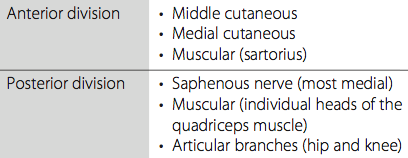 Femoral nerve block results in anesthesia of the skin and muscles of the anterior thigh and most of the femur and knee joint (Figure 4). The block also confers anesthesia of the skin on the medial aspect of the leg below the knee joint (saphenous nerve, a superficial terminal extension of the femoral nerve). Single Injection Femoral Nerve Block Equipment A standard regional anesthesia tray is prepared with the following equipment:
Landmarks and Patient Positioning The patient is in the supine position with both legs extended. In obese patients, a pillow placed underneath the hips can facilitate palpation of the femoral artery and the block performance.
A
B Figure 4: (A) Motor innervation of the femoral nerve. (B) Sensory innervation of the femoral nerve and its cutaneous branches. Landmarks for the femoral nerve block are easily recognizable in most patients and include the femoral crease (Figure 5) and femoral artery pulse (Figure 6).
The following maneuvers can be used to facilitate landmark identification:
The needle insertion site is labeled immediately lateral to the pulse of the femoral artery (Figure 6). All landmarks should be outlined with a marking pen.
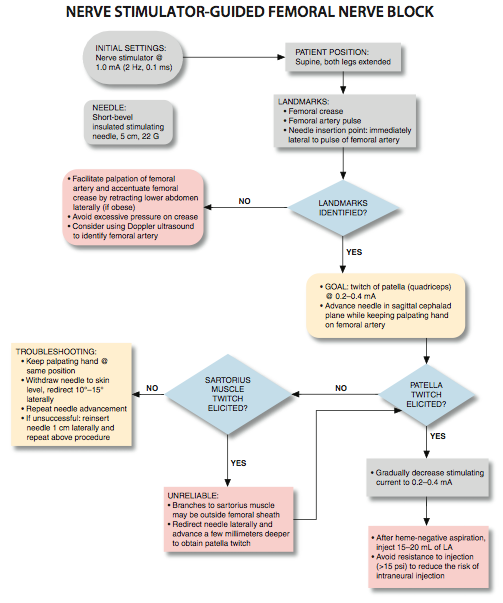
Technique After thorough preparation of the area with an antiseptic solution, local anesthetic is infiltrated subcutaneously at the estimated site of needle insertion. The injection for the skin anesthesia should be shallow and in a line extending laterally to allow for a more lateral needle reinsertion when necessary. The anesthesiologist should stand at the side of the patient with the palpating hand on the femoral artery. The needle is introduced immediately at the lateral border of the artery and advanced in sagittal, slightly cephalad plane (Figure 1). After initial stimulation of the femoral nerve is obtained, the stimulating current is gradually decreased until twitches are still seen or felt at 0.2 to 0.4 mA, which typically occurs at a depth of 2 to 3 cm. After obtaining negative results from an aspiration test for blood, 15 to 20 mL of local anesthetic is injected slowly.
Troubleshooting When stimulation of the quadriceps muscle is not obtained on the first needle pass, the palpating hand should not be moved from its position. Instead, visualize the needle plane in which the stimulation was not obtained and:
When the procedure just described fails to produce a twitch, the needle is withdrawn from the skin and reinserted 1 cm laterally, and the previously described steps are repeated with a progressively more lateral needle insertion. Table 2 shows some common responses to nerve stimulation and the course of action required to obtain the proper response.
Block Dynamics and Perioperative Management Femoral nerve blockade is associated with minimal patient discomfort because the needle passes only through the skin and adipose tissue of the femoral inguinal region. However, many patients feel uncomfortable being exposed during palpation of the femoral artery, and appropriate sedation is necessary for the patient's comfort and acceptance. The administration of midazolam 1 to 2 mg after the patient is positioned and alfentanil 250 to 500 µg just before infiltration of the local anesthetic suffices for most patients. A typical onset time for this block is 15 to 20 minutes, depending on the type, concentration, and volume of anesthetic used. The first sign of onset of the blockade is a loss of sensation in the skin over the medial aspect of the leg below the knee (saphenous nerve). Weightbearing on the blocked side is impaired, which should be clearly explained to the patient to prevent falls. Some practitioners advocate the use of large volume of local anesthetic to anesthetize lateral femoral cutaneous and obturator nerves in addition to the femoral nerve. However, such an extensive spread of the local anesthetic has not been substantiated in the literature. Injection of local anesthetic during femoral nerve blockade results primarily in pooling of the injectate around the femoral nerve underneath the fascia iliaca without consistent lateramedial spread (Figure 8). Continuous Femoral Nerve Block  Figure 7: When lateral redirection of the needle does not bring about motor response, the needle is reinserted 1 cm lateral to the original reinsertion point. The continuous femoral nerve block technique is similar to the single-injection procedure; however, insertion of the needle at a slightly lower angle may be necessary to facilitate threading of the catheter. The most common indications for use of this block are postoperative analgesia after knee arthroplasty, anterior cruciate ligament repair, and femoral fracture repair. Equipment A standard regional anesthesia tray is prepared with the following equipment:
Either nonstimulating (conventional) or stimulating catheters can be used. During the placement of a conventional, nonstimulating catheter, the stimulating needle is first advanced until appropriate motor responses are obtained. Five to 10 mL of local anesthetic or nonconducting injectate (e.g., D5W) is injected to "open up" a space for the catheter to advance with less resistance. Then the catheter is threaded through the needle to approximately 3-5 cm beyond the tip of the needle. The needle is withdrawn, the catheter secured, and the remaining local anesthetic is injected via the catheter. Table 2: Common Responses to Nerve Stimulatin and Course of Action for Proper Response 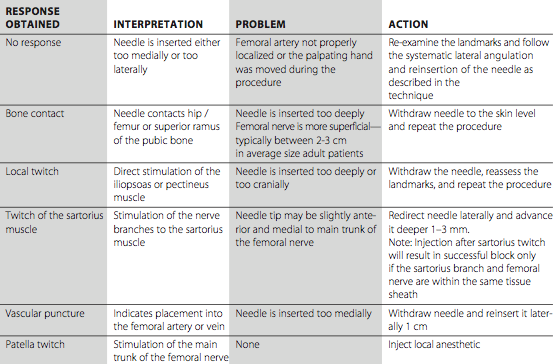 Landmarks and Patient Positioning  Figure 8: Injection of local anesthetic during femoral nerve blockade results primarily in pooling of the injectate around the femoral nerve underneath the fascia iliaca without consistent latera-medial spread. FN - femoral nerve, IC - Iliac Crest, P - Psoas Muscle, I - Iliacus muscle, ON - Obturator Nerve.
Figure 9: Catheter insertion for continuous femoral nerve block. The catheter is inserted 3-5 cm beyond the needle tip. The patient is in the supine position with both legs extended. In obese patients, a pillow placed underneath the hips can facilitate palpation of the femoral artery and the block performance. The landmarks for a continuous femoral block include: 1. Femoral (inguinal crease) 2. Femoral artery 3. Needle insertion site is marked immediately lateral to the pulse of the femoral artery Technique With the patient in the supine position, the skin is infiltrated with local anesthetic at the injection site using a 25-gauge needle. The palpating hand is used to keep the middle finger on the pulse of the femoral artery while the entire hand slightly pulls the skin caudally to keep it from wrinkling on needle insertion (Figure 1). The stimulating needle connected to the nerve stimulator (1.0 mA) is inserted and advanced at a 45° to 60° angle. Care should be taken to avoid insertion of the needle too medially to decrease the risk of a puncture of the femoral artery. The goal is to obtain a quadriceps muscle response (patella twitch) at 0.5 mA. The catheter should be advanced 3 to 5 cm beyond the needle tip (Figure 9). The catheter is advanced deeper in obese patients to prevent catheter dislodgement with shifting of the adipose tissue postoperatively. Then the needle is withdrawn back to the skin level, and the catheter is advanced simultaneously to prevent inadvertent removal of the catheter. The catheter is checked for inadvertent intravascular placement and secured to the thigh using an adhesive skin preparation such as benzoin, followed by application of a clear dressing. The infusion port should be clearly marked "continuous nerve block." Continuous Infusion Continuous infusion is always initiated following an initial bolus (15-20 mL) of dilute local anesthetic through the needle or catheter. For this purpose, we routinely use 0.2% ropivacaine. The infusion is maintained at 5 mL/h with a patient-controlled regional analgesic dose of 5 mL/h. Complications and How to Avoid Them Table 3 provides some general and specific instructions on possible complications and how to avoid them. Table 3: Complications of Femoral Nerve Block and Preventive Techniques 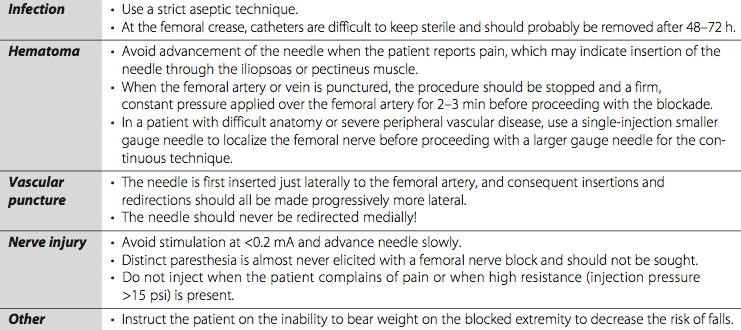
|
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)
























Post your comment