Optimizing an Ultrasound Image
|
Author: Daquan Xu Optimizing an image produced by ultrasound is an essential skill for performance of an ultrasound-guided nerve block. Anatomically, peripheral nerves are often located in the vicinity of an artery or between muscle layers. The echo texture of normal peripheral nerves can have a hyperechoic, hypoechoic, or honeycomb pattern (Figure 1). Several scanning steps and techniques can be used to facilitate ade- quate nerve imaging, including the selection of sonographic modes, adjustment of function keys, needle visualization, and interpretation of image artifacts. All in all, sonographic imaging modes used for ultrasound- guided regional anesthesia and medical diagnostics are conventional imaging, compound imaging, and tissue harmonic imaging (THI). The conventional imaging is generated by a single-element angle beam. The compound imaging is implemented by acquiring several (usually three to nine) overlapping frames from different frequencies or from different angles. The tissue harmonic imaging acquires the information from harmonic frequencies generated by ultrasound beam transmission through tissue, which improves tissue contrast by suppression of scattering signals. Compound imaging with The tissue harmonic imaging can provide images with better resolution, penetration, and interfaces and margin enhancement, compared with those obtained using conventional sonography. In Figure 2, compound imaging and conventional imaging was used to view the interscalene brachial plexus. There is a clear margin definition of two hypoechoic oval-shaped nerve structures in compound imaging. As an example, the contrast resolution between the anterior scalene muscle and the surrounding adipose tissue is enhanced in comparison with those made with conventional imaging techniques. Five function keys on an ultrasound machine are of crucial importance to achieve an optimal image during the performance of peripheral nerve imaging (Figure 3A). 1. Depth: The depth of the nerve is the first consideration when ultrasound-guided nerve block is performed. The depth at which peripheral nerves are positioned and therefore imaged greatly varies and also depends on a patient's habitus. An optimal depth setting is important for proper focusing properties during imaging. Table 1 describes the recommended initial depth settings for common peripheral nerves. The target nerve should be at the center of the ultrasound image to obtain the best resolution of the nerve and reveal other anatomic structures in the vicinity of the nerve. For example, ultrasound imaging during supraclavicular or infraclavicular brachial plexus blockade requires that first rib and pleura are viewed simultaneously to decrease the risk of lung puncture with the needle. 
Figure 1: Architecture of peripheral nerves 
Figure 2: Examples of image quality typically obtained with conventional versus compound imaging. 
Figure 3: Optimizing an ultrasound image using five key functional adjustments (A) and specific tips on adjusting the focus (B) and gain (C). Some ultrasound models are specifically optimized for regional anesthesia application and may not incorporate user-adjustable focus and/or time gain compensation (TGC). 
Figure 3 (Continued) 2. Frequency: The ultrasound transducer with the optimal frequency range should be selected to best visualize the target nerves. Ultrasound energy is absorbed gradually by the transmitted tissue; the higher the frequency of ultrasound, the more rapid the absorption, and the less distance propagation. Therefore, a low-frequency transducer is used to scan structures at a deeper location. Unfortunately, this is at the expense of reduced image resolution. 3. Focusing: Lateral resolution can be improved by choosing the higher frequency as well as by focusing the ultrasound beam. In actual practice, the focus is adjusted at the level of the target nerve; the best image quality for a given nerve is obtained by choosing an appropriate frequency transducer and the focal zone (Figure 3B). Table 1: Suggested Optimal Imaging Depth for Common Peripheral Nerve Blocks 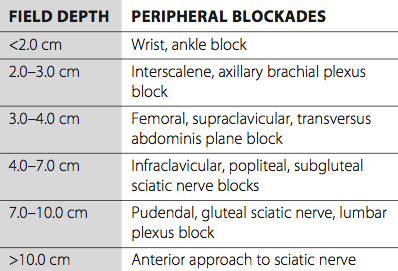 4. Gain: Screen brightness can be adjusted manually by two function buttons: gain and time-gain compensation (TGC). Excessive or inadequate gain can cause both a blurring of tissue boundaries and a loss of information. Optimal gain for scanning peripheral nerves is typically the gain at which the best contrast is obtained between the muscles and the adjacent connective tissue. This is because muscles are well-vascularized tissue invested with connective tissue fibers, whereas, the echo texture of connective tissue is similar to that of nerves. In addition, increasing gain below the focus works well with the TGC control to visualize both the target nerve and the structures below it. Figure 3C shows the same section with both correct and incorrect gain and TGC settings. 5. Doppler: In regional anesthesia, Doppler ultrasound is used to detect vascular structures or the location of the spread of the local anesthetic injection. Doppler velocity is best set between 10 and 20 cm/s to reduce aliasing of color Doppler imaging and artifacts of color. Of note, power Doppler is more sensitive for detecting blood flow than color Doppler. Two needle insertion techniques with relevance to the needle-transducer relationship are commonly used in ultrasound-guided nerve block: the in-plane and out-of-plane techniques (Figure 4). In-plane technique means the needle is placed in the plane of ultrasound beam; as a result, the needle shaft and the tip can be observed in the longitudinal view real time as the needle is advanced toward the target nerve. When the needle is not visualized on the image, the needle advancement should be stopped. Tilting or rotating the transducer can bring the ultrasound beam into alignment with the needle and help with its visualization. Additionally, a subtle, fast needle shake and or injection of small amount of injectate may help depict the needle location. The out-of-plane technique involves needle insertion perpendicularly to the transducer. The needle shaft is imaged in a cross-section plane and can be identified as a bright dot in the image. Visualization of the tip of the needle, however, is difficult and unreliable. The method used to visualize the tip of the needle is as follows: Once a bright dot (shaft) is seen in the image, the needle can be shaken slightly and/or the transducer can be tilted toward the direction of needle insertion simultaneously until the dot disappears. Shaking the needle helps differentiate the echo as emanating from the needle or from the surrounding tissue. The last capture of the hyperechoic dot is its tip. A small amount of injectate can be used to confirm the location of needle tip. Whenever injectate is used to visualize the needle tip, attention must be paid to avoid resistance (pressure) to injection because when the needle–nerve interface is not well seen, there is a risk for an intraneural injection.  Figure 5: In-plane and out-of-plane needle insertion and corresponding ultrasound image. By definition, ultrasound artifact is any image aberration that does not represent the correct anatomic arrangement. The five artifacts often seen in regional anesthesia practice (Figure 5) are as follows. 1. Shadowing is a significant reduction of ultrasound energy lying below solid objects (e.g., osseous structures, gallstone). This is manifested by attenuation of the echo signals as seen in an abnormal decrease of the brightness, which appear as a shadow on the image. 2. Enhancement manifests as overly intense echogenicity behind an object (such as vessel, cyst) that is less attenuating than the surrounding soft tissues. The echo signals are enhanced in brightness disproportional to the echo strength. Scanning from different angles or from different planes may help to decrease shadowing/enhancement artifacts and to visualize the target nerve. 3. Reverberation is a set of equally spaced bright linear echoes behind the reflectors in the near field of the image. It may be attenuated or eliminated when scanning direction is changed or ultrasound frequency is decreased. 4. Mirror Image artifact results from an object located on one side of a highly relfective interface, appearing on the other side of a highly relective interface, appearing on the other side as well. Both virual and artificial images have an equal distance to the relector from opposite direcitons. Changing scanning direction may decrease the artifact. 5. Velocity error is the displacement of the interface, which is caused by the difference of actual velocity of ultrasound in human soft tissue, compared with the calibrated speed, which is assumed to be 1540 m/sec in the ultrasound system. The inherent artifact in the process of scanning cannot be completely eliminated in all cases by manipulating ultrasound devices or changing the settings. However, recognizing and understanding ultrasound artifacts help the operator avoid misinterpretation of images. Here is an acronym, SCANNING, for preparing to scan: S: Supplies C: Comfortable positioning A: Ambiance N: Name and procedure N: Nominate transducer I: Infection control N: Note lateral/medial side on screen G: Gain depth 1. Gather supplies: All equipment necessary for ultrasound scanning should be prepared. Equipment may differ slightly depending on the area to be scanned; however some necessary equipment includes: a. Ultrasound machine b. Transducer covers c. Nerve block kit, nerve stimulator d. Sterile work trolley e. Local anesthetic drawn up and labeled f. Whenever possible, connect the ultrasound machine to the power outlet to prevent the machine from powering down during a procedure 2. Comfortable patient position: Patient should be positioned in such a way that the patient, the anesthesiologist, the ultrasound machine, and the sterile block tray are all arranged in an ergonomic position that allows for a time-efficient performance of the procedure. a. The ultrasound machine should be set up on the opposite side of the patient with the screen at the operator's eye level. b. Block tray should be positioned close enough to the operator so it eliminates the need to reach for needle, gel, and other supplies but should not interfere with the scanning procedure. 3. Ambiance-set room settings: Adjust the lights in the room in order to view the ultrasound machine and procedural site adequately. a. Dim lighting optimizes visualization of the image on the screen; more lighting is typically needed for the procedural site. b. Adjust the room light settings to allow for proper lighting to both areas, as well for safe monitoring of the patient. 4. Name of patient, procedure, and site of procedure: Before performing a scan take a "time-out" to ensure patient information is correct, the operation being done is confirmed, and the side in which the procedure is being done is validated. Checking that patient informati on is entered into the ultrasound machine and matches the information on the patient's wristband not only confirms identity but also allows for images to be saved during the scanning process for documentation. 5. Select transducer: Select the transducer that best fits the scheduled procedure to be done. a. A linear transducer is best scanning superficial anatomic structures; a curved (phased array) transducer displays a sector image and is typically better for deeper positioned structures. 6. Disinfection: Disinfect the patient's skin using a disinfectant solution to reduce the risk of contamination and infection. 
Figure 5: Common artifacts during ultrasound imaging. LA - local anesthetic, MSM - middle scalene muscle. 7. Orient transducer and apply gel: The operator should orient the transducer to match the medial-lateral orientation of the patient. This is conventionally not done by radiologists/sonographers, but it is very useful for intervention-oriented regional anesthesia procedures. a. Touch one edge of the transducer to orient the side of the transducer so the medial-lateral orientation on the patient corresponds to that on the screen. b. A sufficient amount of gel is applied to either the transducer or the patient's skin to allow for transmission of the ultrasound. A copious amount of disinfectant solution can be used instead of gel in many instances. c. Insufficient quality of gel will decrease reflection-absorption rates and may result in unclear/blurry images on the ultrasound image being displayed. 8. Place transducer on the patient's skin and adjust ultrasound machine settings: a. The gain should be adjusted with the general gain setting and/or by using TGC. b. The depth is adjusted to optimize imaging of structures of interest. c. Where available, focus point is adjusted at the desired level. d. Scanning mode can be switched to aid in the recognition of the structures as necessary (e.g., color Doppler can help depict blood vessels, M-mode can distinguish between arteries and veins).  |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../files/bk-nysora-ad.jpg)












Post your comment