Ultrasound-Guided Popliteal Sciatic Block
Figure 1: Cross-sectional anatomy of the sciatic nerve in the popliteal fossa. Shown are common peroneal nerve (CPN), tibial nerve (TN), popliteal artery (PA), popliteal vein (PV), femur, biceps femoris (BFM), semimembranosus (SmM) and semitendinosus (StM) muscles. Essentials
General Considerations Performance of a sciatic block above the popliteal fossa benefits from ultrasound guidance in several ways. The anatomy of the sciatic nerve as it approaches the popliteal fossa can be variable, and the division into the tibial nerve (TN) and common peroneal nerve (CPN) occurs at a variable distance from the crease. Knowledge of the location of the TPN and CPN in relation to each other is beneficial in ensuring the anesthesia of both divisions of the sciatic nerve. Moreover, with nerve stimulator-based techniques, larger volumes (e.g., >40 mL) of local anesthetic often are required to increase the chance of block success and rapid onset. A reduction in local anesthetic volume can be achieved with ultrasound guidance because the injection can be halted once adequate spread is documented. The two approaches to the popliteal sciatic block common in our practice are the lateral approach with patient in supine (more commonly, oblique position) and the posterior approach (Figure 2). It should be noted that with the lateral approach, the resulting ultrasound image is identical to the image in the posterior approach. Both are discussed in this chapter. Only the patient position and needle path differ between the two approaches; the rest of the technique details are essentially the same. Ultrasound Anatomy With the posterior and the lateral approaches, the transducer position is identical; thus the sonographic anatomy appears the same. However, note that although the image appears the same, there is a 180° difference in patient orientation. Beginning with the transducer in the transverse position at the popliteal crease, the popliteal artery is identified, aided with the color Doppler ultrasound when necessary, at a depth of approximately 3 to 4 cm. The popliteal vein accompanies the artery. On either side of the artery are the biceps femoris muscles (lateral) and the semimembranosus and semitendinosus muscles (medial). Superficial (i.e., toward the skin surface) and lateral to the artery is the tibial nerve, seen as a hyperechoic, oval, or round structure with a stippled or honeycomb pattern on the interior (Figure 3A and B). If difficulty in identifying the nerve is encountered, the patient can be asked to dorsiflex and plantar flex the ankle, which makes the nerve rotate or move in relation to its surroundings. Once the tibial nerve is identified, an attempt can be made to visualize the common peroneal nerve, which is located even more superficial and lateral to the tibial nerve. The transducer should be slid proximally until the tibial and peroneal nerves are visualized coming together to form the sciatic nerve before its division. (Figure 4A and B). This junction usually occurs at a distance between 5 and 10 cm from the popliteal crease but this may occur very close to the crease or (less commonly) more proximally in the thigh. As the transducer is moved proximally, the popliteal vessels move anteriorly (i.e., deeper) and therefore become less visible. Adjustments in depth, gain, and direction of the ultrasound beam should be made to keep the nerve visible at all times. The sciatic nerve typically is visualized at a depth of 2 to 4 cm.
Figure 2: Posterior approach to ultrasound-guided popliteal sciatic block can be performed with the patient in the oblique position (A) or with the patient prone (B).
Distribution of Blockade  Figure 5: Needle insertion technique to block the sciatic nerve in the popliteal fossa using lateral approach with patient in the supine position.
Figure 6: Sonoanatomy of the popliteal fossa imaged with the transducer positioned as in Figure 5. The image appears inverted compared to the image in the lateral/ oblique position. Sciatic nerve block results in anesthesia of the entire lower limb below the knee, both motor and sensory, with the exception of a variable strip of skin on the medial leg and foot, which is the territory of the saphenous nerve, a branch of the femoral nerve. The motor fibers to the hamstring muscles are spared; however, sensory fibers to the posterior aspect of the knee are still blocked. For a more comprehensive review of the sciatic nerve distribution. Equipment A standard regional anesthesia tray is prepared with the following equipment:
Lateral Approach Landmarks and Patient Positioning This block is performed with the patient in the supine or oblique (more convenient) position. Sufficient space must be made to accommodate the transducer beneath the knee and thigh.This can be accomplished either by resting the foot on an elevated footrest or flexing the knee while an assistant stabilizes the foot and ankle on the bed (Figure 5). If nerve stimulation is used at the same time, exposure of the calf and foot are required to observe motor responses.
 Figure 7: Simulated needle path and the proper needle tip placement to block the sciatic nerve (ScN) through the lateral approach. BFM - Biceps femoris muscle, SmM - Semimembranosus muscle. StM - Semitendinosus muscle, PA- Popliteal artery. Technique With the patient in the proper position, the skin is disinfected and the transducer positioned to identify the sciatic nerve (Figure 5). If the nerve is not immediately apparent, tilting the transducer proximally or distally can help improve the contrast and bring the nerve "out" of the background (Figure 6). Alternatively, sliding the transducer slightly proximally or distally may improve the quality of the image and allow for better visualization. Once identified, a skin wheal is made on the lateral aspect of the thigh 2 to 3 cm above the lateral edge of the transducer. Then the needle is inserted in-plane in a horizontal orientation from the lateral aspect of the thigh and advanced toward the sciatic nerve (Figure 7). If nerve stimulation is used (0.5 mA, 0.1 msec), the contact of the needle tip with the sciatic nerve usually is associated with a motor response of the calf or foot. Once the needle tip is witnessed adjacent to the nerve, and after careful aspiration, 1 to 2 mL of local anesthetic is injected to confirm the proper injection site. Such injection should result in distribution of the local anesthetic within the epineural sheath, and often, separation of the TN and CPN. When injection of the local anesthetic does not appear to result in a spread around the sciatic nerve (Figure 8), additional needle repositions and injections may be necessary. When injecting into the epineurium, correct injection is recognized as local anesthetic spread proximally and distally to the site of the injection around both divisions of the nerve. This typically results in separation of TN and CPN during and after the injection.
Figure 8: Simulated needle path and local anesthetic distribution to block the sciatic nerve in the popliteal fossa using the lateral approach. Posterior Approach Landmarks and Patient Positioning This block is performed with the patient in the prone or oblique position with the legs slightly abducted. A small footrest is useful to facilitate identification of a motor response if nerve stimulation is used. Also, it relaxes the hamstring tendons, making transducer placement and manipulation easier. Technique With the patient in the proper position, the skin is disinfected and the transducer positioned to identify the sciatic nerve (Figure 2). Similar maneuvers as described for the lateral approach can be made to better visualize the nerve. Once identified, a skin wheal is made immediately lateral or medial to the transducer. Then the needle is inserted in plane and advanced toward the sciatic nerve (Figures 9 and 10). If nerve stimulation is used (0.5 mA, 0.1 msec), the contact of the needle tip with the sciatic nerve often is associated with a motor response of the calf or foot. Once the needle tip is confirmed to be adjacent to the nerve, the syringe is gently aspirated and the local anesthetic deposited. Needle repositioning and injection of smaller aliquots is frequently required to ensure adequate circumferential spread of the local anesthetic (Figure 11).
 Figure 9: Transducer position and in-plane needle insertion to block the sciatic nerve at the popliteal fossa with patient in prone position. Continuous Ultrasound-Guided Popliteal Sciatic Block The goal of the continuous popliteal sciatic block is to place the catheter in the vicinity of the sciatic nerve within the popliteal fossa. The procedure consists of three phases: needle placement, catheter advancement, and securing the catheter. For the first two phases of the procedure, ultrasound can be used to ensure accuracy in most patients. Typically, the needle is inserted in the same manner as described for the single-shot blocks. An in-plane approach, however, is favored in our practice for the catheter technique because it allows for monitoring of the catheter placement (Figure 12). Proper placement of the needle can be confirmed by obtaining a motor response of the calf or foot, at which point 4 to 5 mL of local anesthetic is injected. This small dose of local anesthetic can make advancement of the catheter easier. The second phase of the procedure involves maintaining the needle in the proper position and inserting the catheter 2 to 4 cm into the space surrounding the sciatic nerve. Insertion of the catheter can be accomplished by either a single operator or with an assistant. Proper position of the catheter is assured by an injection through the catheter and confirming the location and distribution of the injectate and/or monitoring catheter insertion on ultrasound real-time.

Figure 12: Continuous sciatic block in the popliteal fossa using a lateral approach with patient in the supine position. The needle is positioned within the epineural sheath of the sciatic nerve. After an injection of a small volume of local anesthetic to confirm the needle position a catheter is inserted 2-4 cm past the needle tip. Pre-loading the catheter is useful in facilitating the procedure.. The catheter is secured by either taping it to the skin or tunneling. There is no agreement among clinicians regarding what constitutes the ideal catheter securing system. Some clinicians prefer one method over the other. However, the decision regarding which method to use could be based on the patient's age, duration of the catheter therapy, and anatomy. The lateral approach may have some advantage over the prone approach with regard to catheter placement. First, the biceps femoris muscle tends to stabilize the catheter and decrease the chance of dislodgment, compared with the subcutaneous tissue of the popliteal fossa in the prone approach. Second, if the knee is to be flexed and extended, the side of the thigh is less mobile than the back of the knee. Finally, access to the catheter site is more convenient with the lateral approach compared with the prone approach. A commonly suggested starting infusion regimen is to infuse ropivacaine 0.2% at 5 mL/hour with a patient-delivered bolus of 5 mL every 60 minutes.  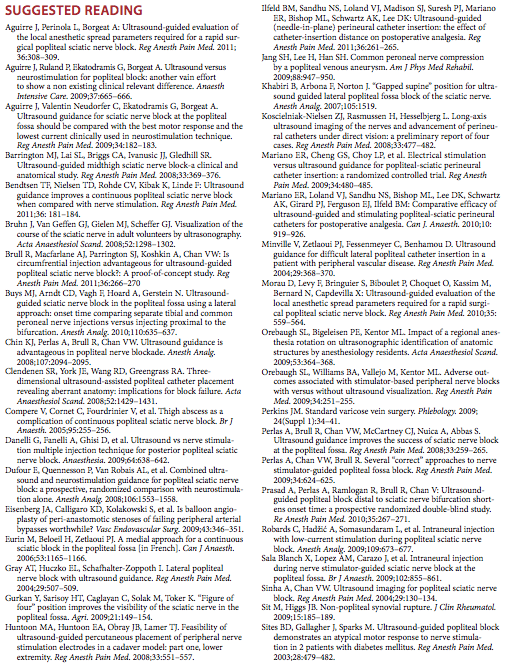 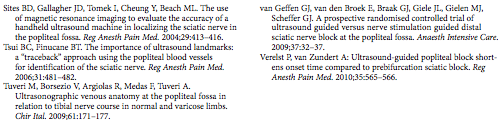 |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)

























Post your comment