Intertendinous / Lateral Approach
|
A
B Figure 1-1: (A) Needle insertion for the popliteal intertendinous approach. (B) Needle insertion for lateral approach to popliteal block. Essentials
PART 1: INTERTENDINOUS APPROACH General Considerations The popliteal block is a block of the sciatic nerve at the level of the popliteal fossa. This block is one of the most useful blocks in our practice. Common indications include corrective foot surgery, foot debridement, and Achilles tendon repair. A sound knowledge of the principles of nerve stimulation and the anatomic characteristics of the connective tissue sheaths of the sciatic nerve in the popliteal fossa are essential for its successful implementation. Functional Anatomy The sciatic nerve is a nerve bundle consisting of two separate nerve trunks, the tibial and the common peroneal nerves (Figure 1-2). A common epineural sheath envelops these two nerves at their outset in pelvis. As the sciatic nerve descends toward the knee, the two components eventually diverge in the popliteal fossa to continue their paths separately as the tibial and the common peroneal nerves. This division of the sciatic nerve usually occurs between 4 and 10 cm proximal to the popliteal fossa crease. From its divergence from the sciatic nerve, the common peroneal nerve continues its path downward and laterally, descending along the head and neck of the fibula, Figure 1-2. Its major branches in this region are branches to the knee joint and cutaneous branches to the sural nerve. Its terminal branches are the superficial and deep peroneal nerves. The tibial nerve is the larger of the two divisions of the sciatic nerve. It continues its path vertically through the popliteal fossa, and its terminal branches are the medial and lateral plantar nerves, Figure 1-2. Its collateral branches give rise to the medial cutaneous sural nerve, muscular branches to the muscles of the calf, and articular branches to the ankle joint. It is important to note that the sciatic nerve in the popliteal fossa is lateral and superficial to the popliteal artery and vein, and it is contained in its own tissue (epineural) sheath rather than in a common neurovascular tissue sheath. This anatomic characteristic explains the relatively low risk of systemic toxicity and vascular punctures with a popliteal block (Figure 1-3). However, the proximity of the large vessels, popliteal artery, and vein still makes it imperative to carefully rule out an intravascular needle placement by careful aspiration and meticulously slow injection (e.g., ≤20 mL/min). 
Figure 1-2: Anatomy of the sciatic nerve in the popliteal fossa. The sciatic nerve (1) is shown with its two divisions, tibial (2) and common peroneal(3) nerves. The common sciatic nerve is is seen between semitendinosus ((4), medially) and biceps ((5), laterally) muscles enveloped by the thick epineural sheath (6). Distribution of Blockade 
Figure 1-3: The spread of the contrast solution after injection into the common epineural sheath of the sciatic nerve (SN). The sciatic nerve is positioned between the biceps femoris (BF) and semimembranosus (SM) muscles. An extensive spread within the epineural sheath is seen. A popliteal block results in anesthesia of the entire distal two thirds of the lower leg, with the exception of the skin on the medial aspect. Cutaneous innervation of the medial leg below the knee is provided by the saphenous nerve, a cutaneous terminal extension of the femoral nerve. When the surgery is on the medial aspect of the leg, the addition of a saphenous nerve block or local anesthetic infiltration at the incision site may be required for complete anesthesia. Popliteal block alone is usually sufficient for tourniquet on the calf because the tourniquet discomfort is the result of pressure and ischemia of the deep muscle beds and not of the skin and subcutaneous tissues. Technique Equipment A standard regional anesthesia tray is prepared with the following equipment:
Landmarks and Patient Positioning The patient is in the prone position. The foot on the side to be blocked should be positioned so that even the slightest movements of the foot or toes can be easily observed. This is best achieved by allowing the foot to extend beyond the operating room bed. 
Figure 1-4: Landmarks for the popliteal block. (1) popliteal fossa crease. (2) biceps femoris tendon. (3) semitendinosus semimembranous muscles.
Landmarks for the intertendinous approach to a popliteal block are easily recognizable even in obese patients (Figure 1-4): 1. Popliteal fossa crease 2. Tendon of the biceps femoris muscle (latearlly) 3. Tendons of the semitendinosus and semimembranosus (medially) Maneuvers to Facilitate Landmark Identification The anatomic structures are best accentuated by asking the patient to elevate the foot while palpating muscles against resistance. This allows for easier and more reliable identification of the hamstring tendons. All three landmarks should be outlined with a marking pen. The needle insertion point is marked at 7 cm above the popliteal fossa crease at the midpoint between the two tendons (Figure 1-5).
Technique 
Figure 1-7: The needle is re-oriented laterally when the contractions of the local twitches of the semitendinosus and semimembranous muscles are elicited. After a thorough cleaning of the injection site with an antiseptic solution, local anesthetic is infiltrated subcutaneously. The anesthesiologist stands at the side of the patient with the palpating hand on the biceps femoris muscle. The needle is introduced at the midpoint between the tendons (Figure 1-6). This position allows the anesthesiologist to both observe the responses to nerve stimulation and monitor the patient. The nerve stimulator should be initially set to deliver a current of 1.5 mA (2 Hz, 0.1 ms) because this higher current allows the detection of inadvertent needle placement into the hamstring muscles (local twitches). When the needle is inserted in the correct plane, its advancement should not result in any local muscle twitches; the first response to nerve stimulation is typically that of the sciatic nerve (a foot twitch). After initial stimulation of the sciatic nerve is obtained, the stimulating current is gradually decreased until twitches are still seen or felt at 0.2 to 0.5 mA. This typically occurs at a depth of 3 to 5 cm. After obtaining negative results from an aspiration test for blood, 30 to 40 mL of local anesthetic is slowly injected.
Figure 1-8: The needle is re-oriented medially when local twitches of the biceps femoris muscle are elicited. Troubleshooting When insertion of the needle does not result in stimulation of the sciatic nerve (foot twitches), implement the following maneuvers: 1. Keep the palpating hand in the same position. 2. Witchdraw the needle to skin level, redirect it 15° laterally, and reinsert it. 3. When step 2 fail to result in sciatic nerve stimulation, withdraw the needle to skin level, reinsert it 1 cm laterally, and repeat the procedure first with perpendicular needle insertion. 4. When step 3 fails, reinsert the needle 15° laterally. These maneuvers should facilitate localization of the sciatic nerve when it proves to be challenging. Table 1-1 lists some common responses to nerve stimulation and the course of action to take to obtain the proper response. Block Dynamics and Perioperative Management This technique is associated with minor patient discomfort because the needle passes only through the adipose tissue of the popliteal fossa. Administration of midazolam 1 to 2 mg after the patient is positioned and alfentanil 250 to 500 µg just before block placement suffice as premedication for most patients. A typical onset time for this block is 15 to 30 minutes, depending on the type, concentration, and volume of local anesthetic used. The first signs of the onset of blockade are usually reports by the patient's of inability to move their toes or that the foot "feels different." With this block, sensory anesthesia of the skin is often the last to develop. Inadequate skin anesthesia despite the apparently timely onset of the blockade is common and it may take up to 30 minutes to develop. Thus local infiltration by the surgeon at the site of the incision is often all that is needed to allow the surgery to proceed.
Table 1-1 Common Responses to Nerve Stimulation and the Course of Action to Obtain the Proper Response 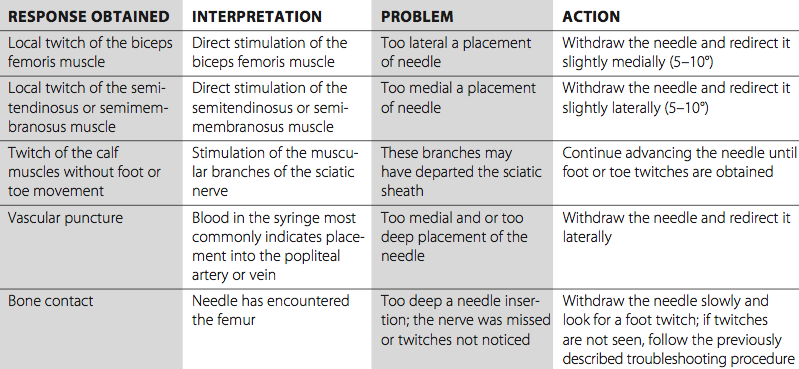
Continuous Popliteal Block The technique is similar to a single-injection procedure; however, slight angulation of the needle cephalad is necessary to facilitate threading the catheter. Securing and maintaining the catheter is easy and convenient. This technique can be used for surgery and postoperative pain management in patients undergoing a wide variety of lower leg, foot, and ankle surgeries. Equipment A standard regional anesthesia tray is prepared with the following equipment:
Kits come in two varieties based on catheter construction: nonstimulating (conventional) and stimulating catheters. During the placement of a conventional nonstimulating catheter, the stimulating needle is first advanced until appropriate twitches are obtained. Then 5-10 mL of local anesthetic or other injectate (e.g., D5W) is then injected to "open up" a space for the catheter to advance freely without resistance. The catheter is then threaded through the needle until approximately 3 to 5 cm is protruding beyond the tip of the needle. The needle is then withdrawn, the catheter secured, and the remaining local anesthetic injected via the catheter. Stimulating catheters are insulated and have a filament or core that transmits current to a bare metal tip. After obtaining twitches with the needle, the catheter is advanced with the nerve stimulator connected until the sought motor response is obtained. This method requires that no conducting solution (i.e., local anesthetic, saline) be injected through the needle prior to catheter advancement, or difficulty obtain- ing a motor response will result. Landmarks and Patient Positioning 
Figure 1-9: Needle direction and insertion of the catheter for continuous popliteal sciatic block. The catheter is inserted 3-5 cm beyond the needle tip. The patient is positioned in the prone position with the feet extending beyond the table to facilitate monitoring of foot or toe responses to nerve stimulation. The landmarks for a continuous popliteal block are essentially the same as those for the single-injection technique (Figure 1-4). These include the following: 1. Popliteal fossa crease 2. Tendon of the biceps femoris muscle (laterally) 3. Tendons of the semitendinosus and semimembranosus The needle insertion site is marked 7 cm proximal to the popliteal fossa crease and between the tendons of the biceps femoris and semitendinosus muscles (Figure 1-5). Technique The continuous popliteal block technique is similar to the single-injection technique. With the patient in the prone position, infiltrate the skin with local anesthetic using a 25-gauge needle at an injection site 7 cm above the popliteal fossa crease and between the tendons of biceps femoris and semitendinosus muscles. An 8- to 10-cm needle connected to the nerve stimulator (1.5 mA current) is inserted at the midpoint between the tendons of the biceps femoris and semitendinosus muscles. Advance the block needle slowly in a slightly cranial direction while observing the patient for rhythmic plantar or dorsiflexion of the foot or toes. After appropriate twitches are noted, continue manipulating the needle until the desired response is seen or felt using a current ≤0.5 mA. The catheter should be advanced no more than 5 cm beyond the needle tip (Figure 1-9). The needle is then withdrawn back to skin level while advancing the catheter simultaneously to prevent inadvertent removal of the catheter. The catheter is checked for inadvertent intravascular placement and secured using an adhesive skin preparation, followed by application of a clear dressing. The infusion port should be clearly marked "continuous nerve block." Continuous Infusion Continuous infusion is initiated after injection of an initial bolus of local anesthetic through the catheter or needle. For this purpose, we routinely use 0.2% ropivacaine 15 to 20 mL. Diluted bupivacaine or levobupivacaine are also suitable but may result in greater degree of motor blockade. The infusion is maintained at 5 to 10 mL/h with a 5-mL patient-controlled bolus hourly.
Complications and How to Avoid Them Complications following a popliteal block are uncommon. Table 1-2 lists some general and specific instructions on possible complications and how to avoid them. Table 1-2: Complications of Popliteal Sciatic Nerve Block and Preventive Techniques 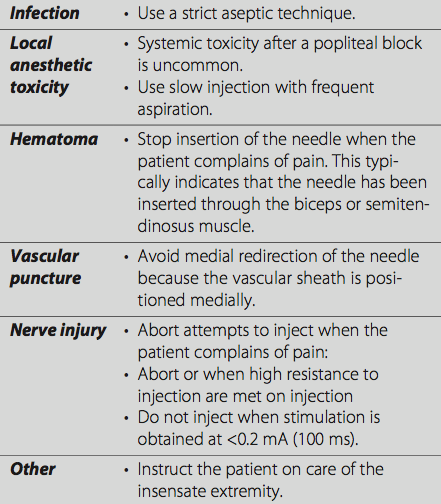 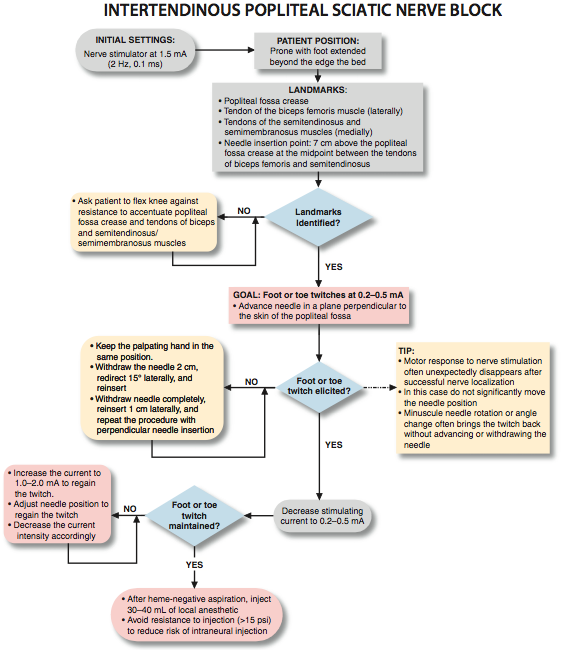   PART 2: LATERAL APPROACH General Considerations The lateral approach to a popliteal blockade is similar to the intertendinous block in many aspects. The main difference is that the technique involves placement of the needle from the lateral aspect of the leg, therefore obviating the need to position the patient in the prone position. Nerve stimulation principles, volume requirements, and block onset time are the same. The block is well suited for surgery on the calf, Achilles tendon, ankle, and foot. It also provides adequate analgesia for a calf tourniquet. Functional Anatomy The sciatic nerve consists of two separate nerve trunks, the tibial and common peroneal nerves (Figure 2-1). A common epineural sheath envelops these two nerves at their outset in the pelvis. As the sciatic nerve descends toward the knee, the two components eventually diverge in the popliteal fossa, giving rise to the tibial and common peroneal nerves. This division of the sciatic nerve usually occurs 5-7 cm proximal to the popliteal fossa crease.
Distribution of Blockade The lateral approach to popliteal block also results in anesthesia of the entire distal two thirds of the lower extremity with the exception of the skin on the medial aspect of the leg (Figure 2-2). Cutaneous innervation of the medial leg below the knee is provided by the saphenous nerve, the terminal extension of the femoral nerve. Depending on the level of surgery, the addition of a saphenous nerve block may be required for complete surgical anesthesia. Single Injection Popliteal Block (Lateral Approach) Equipment A standard regional anesthesia tray is prepared with the following equipment:
Landmarks and Patient Positioning The patient is in the supine position. The foot on the side to be blocked should be positioned so that the motor response of the foot or toes can be easily observed (Figure 2-3). This is best achieved by placing the leg on a footrest with the heel and the foot protruding beyond the footrest. This positioning allows for easy visualization of foot twitches during nerve localization. The foot should form a 90° angle to the horizontal plane of the table. 
Figure 2-1: Anatomy of the popliteal fossa crease. (1) tibial nerve. (2) common peroneal nerve before its division. (3) epineural sheath of the common sciatic nerve. (4) tendon of semitendinosus and semimembranous. (5) bicep femoris tendon. Landmarks for the lateral approach to a popliteal block include the following (Figure 2-4 and 2-5): 1. Popliteal fossa crease 2. Vastus lateralis muscle 3. Biceps femoris muscle The needle insertion site is marked in the groove between the vastus lateralis and biceps femoris muscles 7-8 cm above the popliteal fossa crease. Note that the lateral femoral epicondyle is another landmark that can be used with this technique. It is easily palpated on the lateral aspect of the knee 1 cm cephalad to the popliteal fossa crease (Figures 2-6 and 2-7). 
Figure 2-2: Sensory distribution of anesthesia accomplished with popliteal sciatic block. All shaded areas except medial aspect of the leg (blue, saphenous nerve) are anesthetized with the popliteal block. Maneuvers to Facilitate Landmark Identification Landmarks can be better appreciated using the following steps:
Technique The operator should be seated facing the side to be blocked. The height of the patient's bed is adjusted to allow for a more ergonomic position and greater precision during block placement. This position also allows the operator simultaneously to monitor both the patient and the responses to nerve stimulation. The site of estimated needle insertion is prepared with an antiseptic solution and infiltrated with local anesthetic using a 25-gauge needle. It is useful to infiltrate the skin along a line rather than raise a single skin wheal. This allows needle reinsertion at a different site when necessary without the need to anesthetize the skin again. A 10-cm, 21-gauge needle is inserted in a horizontal plane perpendicular to the long axis of the leg between the vastus lateralis and biceps femoris muscles (Figure 2-8), and it is advanced to contact the femur. Contact with the femur is important because it provides information about the depth of the nerve (typically 1-2 cm beyond the skin to femur distance) and about the angle at which the needle must be redirected posteriorly to stimulate the nerve (Figure 2-9). The current intensity is initially set at 1.5 mA. With the fingers of the palpating hand firmly pressed and immobile in the groove, the needle is withdrawn to the skin level, redirected 30° below the horizontal plane, and advanced toward the nerve. After initial stimulation of the sciatic nerve is obtained, the stimulating current is gradually decreased until twitches are still seen or felt at 0.2-0.5 mA. This typically occurs at a depth of 5-7 cm. At this point, the needle should be stabilized and, after aspiration test for blood, 30-40 mL of local anesthetic is injected slowly.
Troubleshooting 
Figure 2-9: Needle insertion strategy for lateral approach to popliteal sciatic block. (A) needle is first inserted to contact femur. (B) After contact with the femur, the needle is withdrawn back to the skin and redirected 30° posteriorly to local the sciatic nerve. Note the needle passage through the biceps femoris muscle before entering the popliteal fossa crease. This explains why local bicep femoris muscle twitch is often obtained during needle advancement. 1 - Semimembranosus-semitendinosus muscles, 2 - Biceps Femoris, 3 - Femur, 4 - Popliteal artery and vein, 5 - Common peroneal nerve, 6 - TIbial nerve When the sciatic nerve is not localized on the first needle pass, the needle is withdrawn to the skin level and the following algorithm is used: 1. Ensure that the nerve stimulator is functional, properly connected to the patient and to the needle, and set to deliver the current of desired intensity. 2. Ensure that the leg is not externally rotated at the hip joint and that the foot forms a 90° angle to the horizontal plane of the table. A deviation from this angle changes the relationship of the sciatic nerve to the femur and the biceps femoris muscle. 3. Mentally visualize the plane of the initial needle insertion and redirect the needle in a slightly posterior direction (5-10° posterior angulation). 4. If step 3 fails, withdraw the needle and reinsert it with an additional 5-10° posterior redirection. 5. Failure to obtain a foot response to nerve stimulation should prompt reassessment of the landmarks and leg position. In addition, the stimulating current should be increased to 2 mA. Table 2-1 lists the common responses that can occur during block placement using a nerve stimulator and the proper course of action needed to obtain twitches of the foot.
Block Dynamics and Perioperative Management This technique may be associated with patient discomfort because the needle transverses the biceps femoris muscle, and adequate sedation and analgesia are necessary. Administration of midazolam (2-4 mg intravenously) and a short-acting narcotic (alfentanil 250-to 750 g) ensures patient comfort and prevents patient movement during needle advancement. Inadequate premedication can make it difficult to interpret the response to nerve stimulation because of patient movement during needle advancement. A typical onset time for this block is 15-30 minutes, depending on the type, concentration, and volume of local anesthetic used. The first signs of onset of the blockade are usually a report by the patient that the foot "feels different" or there is an inability to wiggle their toes. With this block, sensory anesthesia of the skin is often the last to develop. Inadequate skin anesthesia despite an apparently timely onset of the blockade is common, and it can take up to 30 minutes to develop. Local infiltration by the surgeon at the site of the incision is often all that is needed to allow the surgery to proceed. Continuous Popliteal Block (Lateral Approach) The technique is similar to the single-injection except that slight angulation of the needle cephalad is necessary to facilitate threading of the catheter. Securing and maintaining the catheter are easy and convenient with this technique. A lateral popliteal block is suitable for surgery and postoperative pain management in patients undergoing a wide variety of lower leg, foot, and ankle surgeries. Equipment A standard regional anesthesia tray is prepared with the following equipment:
Either nonstimulating (conventional) or stimulating catheters can be used. During the placement of a conventional non-stimulating catheter, the stimulating needle is advanced until appropriate twitches are obtained. Then 5-10 mL of local anesthetic or other injectate (e.g., D5W) is then injected Table 2-1: Some Common Responses to Nerve Stimulation and Course of Action 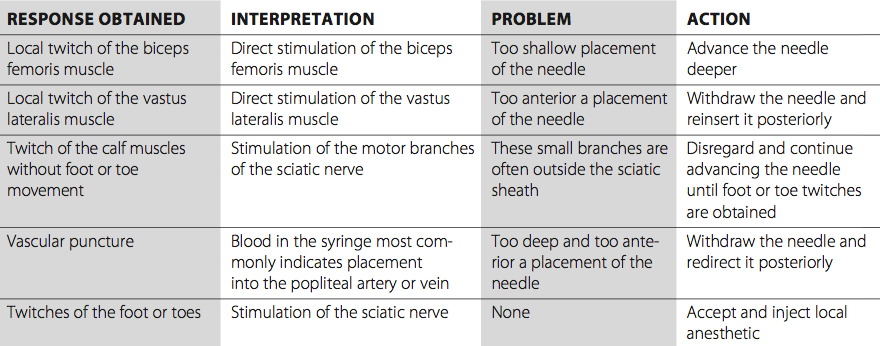 
Figure 2-10: Motor responses of the foot obtained with stimulation of the sciatic nerve in the popliteal fossa. Stimulation of the tibial nerve results in plantar flexion and inversion of the foot. Stimulation of the common peroneal nerve results in dorsi flexion and inversion of the foot. to "open up" a space for the catheter to advance freely with- out resistance. The catheter is threaded through the needle until approximately 3-5 cm is protruding beyond the tip of the needle. The needle is withdrawn, the catheter secured, and the remaining local anesthetic injected via the catheter. With stimulating catheters, after obtaining desired motor response with stimulation through the needle, the catheter is advanced with the nerve stimulator connected until the anesthesiologist is satisfied with the quality of the motor response. If the response is lost, the catheter can be withdrawn until it reappears and the catheter readvanced. This method requires that no conducting solution be injected through the needle (i.e., local anesthetic, saline) prior to catheter advancement, or difficulty obtaining a motor response will result. Landmarks and Patient Positioning The patient is positioned in the supine position with the feet extending beyond the table to facilitate monitoring of foot or toe responses to nerve stimulation. The landmarks for a continuous popliteal block with the lateral approach are essentially the same as for the single-injection technique and include the following: 1. Popliteal fossa crease 2. Vastus lateralis 
Figure 2-11: Catheter insertion technique for popliteal sciatic block. Technique is similar to that of the single-injection technique. Catheter is inserted 3-5 cm beyond the needle tip. 3. Biceps femoris The needle insertion site is marked at 8 cm proximal to the popliteal fossa crease in the groove between the vastus lateralis and biceps femoris. Technique The continuous popliteal block technique is similar to the single-injection technique. The patient is in the supine position. Using a 25-gauge needle, infiltrate the skin with local anesthetic at the injection site 7-8 cm proximal to the popliteal crease in the groove between the biceps femoris and vastus lateralis muscles. An 8- to 10-cm needle with a Tuohy-style tip for a continuous nerve block is connected to the nerve stimulator (1.5 mA) and inserted to contact the femur (Figure 2-11). A slight cephalad orientation to the needle with the opening facing proximally will aid in catheter threading. Once the femur is contacted, the needle is withdrawn to the skin level and redirected in a slightly posterior direction 30°. Then it is advanced slowly while observing the patient for plantar flexion or dorsiflexion of the foot or toes. After obtaining the appropriate twitches, continue manipulating the needle until the desired response is still seen or felt using a current of 0.2-0.5 mA. The catheter should be advanced no more than 5 cm beyond the needle tip. The needle is withdrawn back to the skin level, and the catheter advanced simultaneously to prevent inadvertent removal of the catheter. The catheter is checked for inadvertent intravascular placement and secured to the lateral thigh using an adhesive skin preparation such as benzoin, followed by application of a clear dressing. The infusion port should be clearly marked "continuous nerve block."
Continuous Infusion Continuous infusion is initiated after an initial bolus of dilute local anesthetic is administered through the catheter or needle. For this purpose, we routinely use 0.2% ropivacaine 15-20 mL. Diluted bupivacaine or levobupivacaine are suitable but can result in additional motor blockade. The infusion is maintained at 5 mL/h with 5-mL/h patient-controlled regional analgesia. Complications and How to Avoid Them Table 2-2 provides specific instructions on some complications and how to avoid them.
Table 2-2: Complications of Popliteal Block Through the Lateral Approach and Preventive Techniques 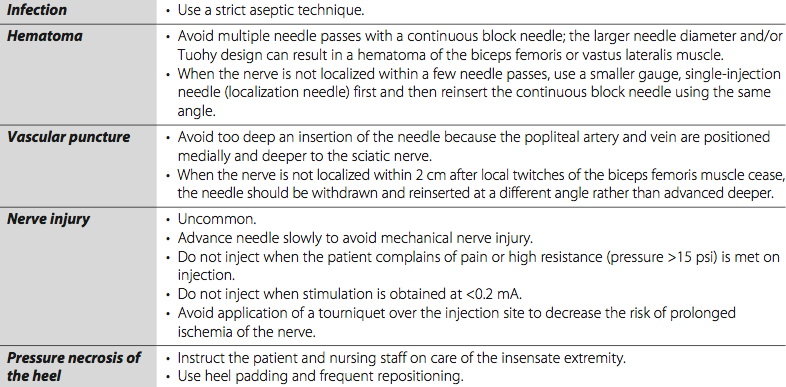 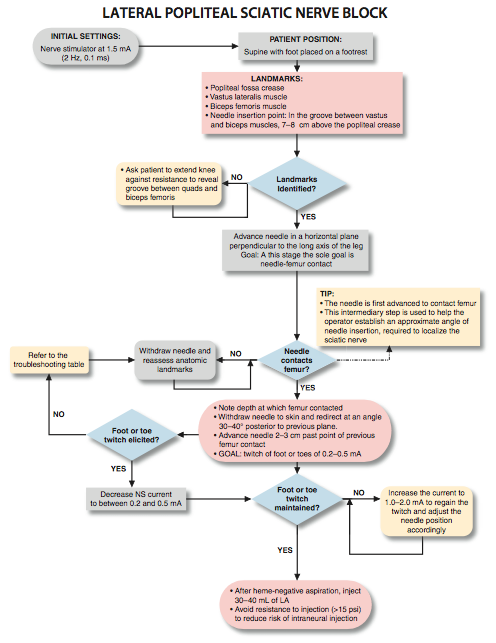  |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)





































Post your comment