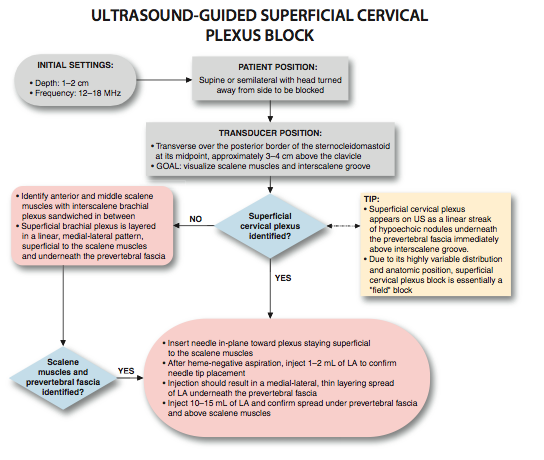
Ultrasound-Guided Superficial Cervical Plexus Block
|
Figure 1: Needle and transducer position to block the superficial cervical plexus using a transverse view. Essentials
General Considerations  Figure 2: Anatomy of the superficial cervical plexus. 1.Sternocleidomastoid muscle;2.mastoid process;3.clavicle;4.external jugular vein. Superficial cervical plexus is seen emerging behind the posterior border of the sternocleidomastoid muscle at the intersection of the muscle with the external jugular vein. 5.Greater auricular nerve. The goal of the ultrasound-guided technique of superficial cervical plexus block is to deposit local anesthetic in the vicinity of the sensory branches of the nerve roots C2, C3, and C4. Advantages over the landmark-based technique include the ability to ensure the spread of local anesthetic in the correct plane and therefore increase the success rate and avoid too deep needle insertion and/or inadvertent puncture of neighboring structures. Both in-plane and out-of-plane approaches can be used. The experience with ultrasound-guided deep cervical plexus is still in its infancy and not described here. Ultrasound Anatomy The sternocleidomastoid muscle (SCM) forms a roof over the nerves of the superficial cervical plexus (C2-4). The roots combine to form the four terminal branches (lesser occipital, greater auricular, transverse cervical, and supraclavicular nerves) and emerge from behind the posterior border of the SCM (Figure 2). The plexus can be visualized as a small collection of hypoechoic nodules (honeycomb appearance or hypo-echoic [dark] oval structures) immediately deep or lateral to the posterior border of the SCM (Figure 3), but this is not always apparent. Occasionally, the greater auricular nerve is visualized (Figure 4) on the superficial surface of the SCM muscle as a small, round hypoechoic structure. The SCM is separated from the brachial plexus and the scalene muscles by the prevertebral fascia, which can be seen as a hyperechoic linear structure. The superficial cervical plexus lies posterior to the SCM muscle, and immediately underneath the prevertebral fascia overlying the interscalene groove. (Figure 3).
Distribution of Blockade The superficial cervical plexus block results in anesthesia of the skin of the anterolateral neck and the anteauricular and retroauricular areas, as well as the skin overlying and immediately inferior to the clavicle on the chest wall (Figure 5).
Equipment Equipment needed includes the following:
Landmarks and Patient Positioning Any patient position that allows for comfortable placement of the ultrasound transducer and needle advancement isappropriate. This block is typically performed in the supine or semi-sitting position, with the head turned slightly away from the side to be blocked to facilitate operator access (Figure 6A and B). The patient's neck and upper chest should be exposed so that the relative length and position of the SCM can be assessed.
Figure 6: Superficial cervical plexus block. A) Transverse approach with an in-plane needle advancement. B) Longitudinal approach.
Goal The goal is to place the needle tip immediately afjacent to the superficial cervial plexus. If it is not easily visualized, the local anesthetic can be deposited in the plane immediately deep to the SC: and inderneath the prevertebral fascia. A volume of 10 to 15 ml of local anesthetic usually suffices. Technique With the patient in the proper position, the skin is disinfected and the transducer is placed on the lateral neck, overlying the SCM at the level of its midpoint (approximately the level of the cricoid cartilage). Once the SCM is identified, the transducer is moved posteriorly until the tapering posterior edge is positioned in the middle of the screen. At this point, an attempt should be made to identify the brachial plexus and/or the interscalene groove between the anterior and middle scalene muscles. The plexus is visible as a small collection of hypoechoic nodules (honeycomb appearance) immediately underneath the prevertebral fascia that overlies the interscalene groove (Figures 3 and 4).
 Figure 11: Desired spread of the local anesthetic under the cervical fascia to block the cervical plexus (CP).
Once identified, the needle is passed through the skin, platysma and prevertebral fascia, and the tip placed adjacent to the plexus (Figure 7). Because of the relatively shallow position of the target, both in-plane (from medial or lateral sides) and out-of-plane approaches can be used. Following negative aspiration, 1 to 2 mL of local anesthetic is injected to confirm the proper injection site. Then the remainder of the local anesthetic (10-15mL) is administered to envelop the plexus (Figure 8). If the plexus is not visualized, an alternative substernocleidomastoid approach can be used. In this case, the needle is passed behind the SCM and the tip is directed to lie in the space between the SCM and the prevertebral fascia, close to the posterior border of the SCM (Figures 6B, 9, and 10). Local anesthetic (10-15 mL) is administered and should be visualized layering out between the SCM and the underlying prevertebral fascia (Figure 11). If injection of the local anesthetic does not appear to result in an appropriate spread, additional needle repositioning and injections may be necessary. Because the superficial cervical plexus is made up of purely sensory nerves, high concentrations of local anesthetic are usually not required; 0.25%-0.5% ropivacaine, bupivacaine 0.25%, or lidocaine 1% are examples of good choices.
|
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)
![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)

 Figure 5: Sensory distribution of the cervical plexus and innervation of the lateral aspect of the face.
Figure 5: Sensory distribution of the cervical plexus and innervation of the lateral aspect of the face.

























Post your comment