Ilioinguinal and Iliohypogastric Blocks
|
Introduction "Almost all cases of hernia, with the possible exception of those in young children, could undoubtedly be subjected to the radical operation under local anesthesia." This quote by Harvey Cushing reported in the Annals of Surgery in 1900 illustrates that over 100 years ago the attributes of regional anesthesia for lower abdominal and inguinal surgerywere appreciated. Ilioinguinal and iliohypogastric blocks are among the most frequently used regional blocks performed for these surgical procedures. Postherniorrhaphy pain is moderate to severe and often poorly controlled with opioids as the single modal therapy.(1) Ilioinguinal and iliohypogastric blocks have been shown to significantly reduce pain associated with herniorrhaphy, regardless of whether the blocks are used as the primary anesthetic(2) or for pain control after general(3,4) or spinal(5) anesthesia. Anatomy  Figure 1: Anatomic relationship of the ilioinguinal and genitofemoral nerves. Both the iliohypogastric and ilioinguinal nerves emanate from the first lumbar spinal root. Superomedial to the anterior superior iliac spine, the iliohypogastric and ilioinguinal nerves pierce the transversus abdominus to lie between it and the internal oblique muscles. After traveling a short distance inferomedially, their ventral rami pierce the internal oblique to lie between the internal and external oblique muscles before giving off branches, which pierce the external oblique to provide cutaneous sensation. The iliohypogastric nerve supplies the skin over the inguinal region. The ilioinguinal nerve runs anteroinferiorly to the superficial inguinal ring, where it emerges to supply the skin on the superomedial aspect of the thigh (Figure 1). Of note, the ventral rami of the lower intercostal nerves (T11 and T12) also pierce the transversus abdominus muscle to lie between it and the internal oblique. These latter nerves also supply sensation to the inferior abdominal wall, and block of these nerves as well as the iliohypogastric and ilioinguinal nerves is essential to provide anesthesia for procedures involving the lower abdominal wall. Method of Block 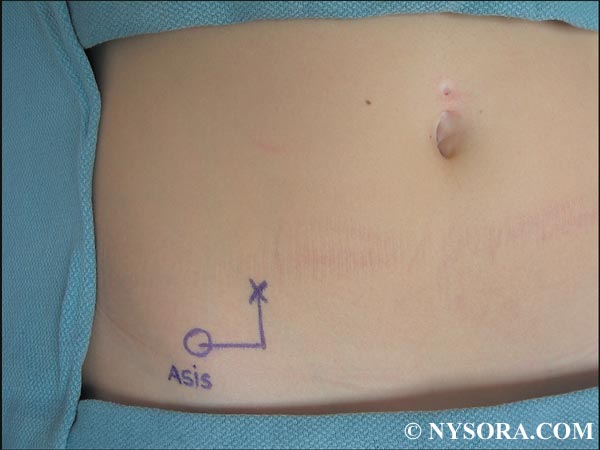 Figure 2: Surface landmarks for ilioinguinal block. The point of needle insertion ismarked 2 cm medial and 2 cm superior from the anterior superior iliac spine. Using the anatomic knowledge previously described, one needs to provide a method of block that allows accurate placement of local anesthetic both between the transversus abdominus and internal oblique muscles as well as between the internal oblique and external oblique muscles. Methods of local anesthetic administration that do not accurately define placement between these muscular layers provide inconsistent anesthesia and analgesia of the abdominal wall and inguinal region. Unfortunately, this may result in the reporting of inadequate analgesia for a procedure that is more a problem of technique than of the block itself.(6) Accurate block techniques must define the specific muscular layers of the abdominal wall. The only way to facilitate this is to use loss of resistance techniques that define fascial layers. Initially, the anterior superior iliac spine is palpated and a mark made 2 cm medial and 2 cm superior from it (Figure 2). After skin preparation and infiltration with local anesthetic, a small puncture is made in the skin with a sharp needle to allow subsequent insertion of a blunt needle. The needle is inserted through the skin puncture site perpendicular to the skin. Increased resistance is met as the needle encounters the external oblique muscle. A loss of resistance is appreciated as the needle passes through the muscle to lie between it and the internal oblique. After the initial loss of resistance and negative needle aspiration for blood, 2 mL of local anesthetic are injected. The needle is then inserted farther to encounter another resistance, which is the internal oblique muscle. 
Figure 3: Needle maneuvers to block to ilioinguoinal nerve. Shown is perpendicular needle insertion (1), lateral (2), and medial (3) redirections (fan technique). A further loss of resistance is appreciated once the needle passes through the internal oblique to lie between it and the transversus abdominus muscle. After the second loss of resistance, another 2 mL of local anesthetic is administered. The needle is then withdrawn to skin and redirected at a 45-degree angle medially to again pierce the external and then the internal oblique muscles (Figure 3). After each loss of resistance, 2 mL of local anesthetic is again administered. The needle is then returned to skin and inserted 45 degrees laterally, and the procedure is repeated. Thus, a total of 12 mL of local anesthetic is placed in a fan-like distribution between the external and internal oblique and the internal oblique and transversus abdominus muscles. Note: In patients with little abdominal wall musculature, the internal oblique muscle may be too thin to appreciate a loss of resistance as it is penetrated. To prevent entering the abdomen (see Complications) after piercing the external oblique muscle, the author limits further abdominal wall penetration without loss of resistance to 1.5 cm. After completion of the block, the skin of the lower abdominal wall or inguinal region is tested for anesthesia. Equipment Any atraumatic needle blunt enough to appreciate a loss of resistance is used for this block. Examples are 22-gauge Whitacre, Sprotte, 18-gauge Tuohy-type (which can also be used to place catheters), 21-gauge Stimuplex needles, etc. Indications and Contraindications Indications for ilioinguinal/iliohypogastric blocks include anesthesia for any somatic procedure involving the lower abdominal wall/inguinal region such as inguinal herniorrhaphy (2-5) and for analgesia after surgical procedures using a Pfannenstiel incision as for cesarean section (7) and abdominal hysterectomy.(8) These blocks do not provide visceral anesthesia and thus cannot be used as the sole anesthetic for procedures such as lower intra-abdominal surgery.When used for inguinal herniorrhaphy, the sac (containing peritoneum) must be infiltrated with local anesthetic by the surgeon to complete anesthesia for the procedure. There are no specific contraindications for these blocks apart from the generic contraindications to performance of any regional block such as infection at the procedure site, allergy to local anesthetics, indeterminate neuropathy, and so on. Choice of Local Anesthetic Unless unusual circumstances occur requiring immediate anesthesia (thus requiring an intermediate-acting agent), a long-acting local anesthetic agent is used to provide the benefits of prolonged postoperative analgesia. We currently use ropivacaine in concentrations of 0.5–1% without adjuvants for ilioinguinal/iliohypogastric blocks (less than 1% concentrations for bilateral blocks such as for Pfannenstiel incisions or bilateral herniorrhaphy). For continuous infusions, ropivacaine in concentrations of 0.2–0.5% is used. Complications and How to Avoid Them Because proper performance of ilioinguinal/iliohypogastric blocks requires multiple small volume injections the possibility of local anesthetic toxicity is remote. Pharmacokinetic studies of 3 mg/kg of 0.5% plain ropivacaine in children revealed peak plasma concentrations of ropivacaine well below the toxic level. (9) A similar study in adults receiving 60–70 mL of 0.5% ropivacaine again revealed low peak plasma concentrations.(10) Because the block is limited to the lower abdominal wall and inguinal region, any hemodynamic changes would be unusual. As with other blocks, the patient is advised to protect the anesthetized area from trauma. Proper performance of ilioinguinal/iliohypogastric blocks places the injection medial and superior to the anterior superior iliac spine. Some texts advocate performing the block from a point medial and inferior to the anterior superior iliac spine, which essentially places the injection within or inferior to the inguinal ligament. This may result in lateral femoral cutaneous or femoral block with little or no ilioinguinal/iliohypogastric anesthesia. However, even properly performed ilioinguinal/iliohypogastric blocks can result in transient femoral anesthesia with a reported incidence of 3.7–5%.(11,12) The mechanism of femoral anesthesia with these methods is tracking of local anesthetic along the fascia iliaca.(13) In the event of femoral anesthesia associated with ilioinguinal/iliohypogastric blocks, the surgeon is notified and the patient is advised to protect the lower extremity until the block recedes. Perforation of both the small (14) and large (15) bowels and creation of a pelvic hematoma (16) have been reported after ilioinguinal/iliohypogastric blocks. This illustrates the importance of using blunt needles to appreciate the loss of resistance as the needle traverses the layers of the abdominal wall. As previously discussed, after piercing the external oblique muscle, limiting further abdominal wall penetration to 1.5 cm should prevent this complication. Continuous Ilioinguinal/Iliohypogastric Blocks Prolonged postoperative analgesia for procedures using a Pfannenstiel incision has been successfully produced using bilateral catheters. Such catheters are an excellent alternative to epidural analgesia by allowing unlimited ambulation without the need for urinary catheterization. Control of visceral pain with NSAIDS or other agents is necessary to complete analgesia. Method From a point 2 cm medial and 2 cm cephalad from the anterior superior iliac spine, an 18-gauge Tuohy-type needle is inserted perpendicular to the skin to pierce the external oblique muscle (see Figure 2). After loss of resistance, a multilumen catheter is inserted and directed medially for 3 inches and secured to skin. The procedure is repeated on the other side. The catheters are either infused using separate pumps or a single pump with flow-restrictor catheters that allow accurate individual catheter flow are used. Individual catheter flow rates of 2 mL/h (0.5% ropivacaine) or 4 mL/h (0.2% ropivacaine) have been used. Summary Regional anesthesia for surgical procedures involving the lower abdomen and inguinal region can be safely and successfully performed using ilioinguinal and iliohypogastric blocks. These techniques accord excellent postoperative analgesia, obviating the need for large-dose opioids and thus facilitating early ambulation and discharge. REFERENCES: 1. Salet G: Patient survey after inguinal hernia repair in ambulatory surgery. Ambulatory Surg 1993;1:194-196. 2. Ding Y, White PF: Post-herniorrhaphy pain in outpatients after preincision ilioinguinal-hypogastric nerve block during monitored anaesthesia care. Can J Anaesth 1995;42:12-15. 3. Harrison CA, Morris S, Harvey JS: Effect of ilioinguinal and iliohypogastric nerve block and wound infiltration with 0.5% bupivacaine on postoperative pain after hernia repair. Br J Anaesth 1994;72:691-693. 4. Bugedo GJ, Carcamo CR, Mertens RA, et al: Preoperative percutaneous ilioinguinal and iliohypogastric nerve block with 0.5% bupivacaine for post-herniorrhaphy pain management in adults. Reg Anesth 1990;15:130-133. 5. Toivonen J, Permi J, Rosenberg PH: Effect of preincisional ilioinguinal and iliohypogastric nerve block on postoperative analgesic requirement in day-surgery patients undergoing herniorrhaphy under spinal anaesthesia. Acta Anaesthesiol Scand 2001;45:603-607. 6. Huffnagle HJ, Norris MC, Leighton BL, Arkoosh VA: Ilioinguinal iliohypogastric nerve blocks-before or after cesarean delivery under spinal anesthesia? Anesth Analg 1996;82(1):8-12. 7. Bell EA, Jones BP, Olufolabi AJ, et al: Women's Anesthesia Research Group. Iliohypogastric-ilioinguinal peripheral nerve block for post-Cesarean delivery analgesia decreases morphine use but not opioidsrelated side effects [English, French]. Can J Anaesth 2002;49(7):694-700. 8. Kelly MC, Beers HT, Huss BK, Gilliland HM: Bilateral ilioinguinal nerve blocks for analgesia after total abdominal hysterectomy. Anaesthesia 1996;51(4):406. 9. Dalens B, Ecoffey C, Joly A, et al: Pharmacokinetics and analgesic effect of ropivacaine following ilioinguinal/iliohypogastric nerve block in children. Paediatr Anaesth 2001;11:415-420. 10. Wulf H, BehnkeH,Vogel I, Schroder J: Clinical usefulness, safety, and plasma concentration of ropivacaine 0.5% for inguinal hernia repair in regional anesthesia. Reg Anesth Pain Med 2001;26(4):348-351. 11. Shandling B, Steward DJ: Regional analgesia for post-operative pain in paediatric outpatient surgery. J Pediatr Surg 1980;15:477-480. 12. Ghani KR,McMillan R, Paterson-Brown S: Transient femoral nerve palsy following ilio-inguinal nerve blockade for day case inguinal hernia repair. J R Coll Surg Edinb 2002;47:626-629. 13. RosarioDJ, Jacob S,Luntley J, et al:Mechanism of femoralnerve palsy complicating percutaneous ilioinguinal field block. Br J Anaesth 1997;78(3):314-316. 14. Amory C, Mariscal A, Guyot E, et al: Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatric Anaesth 2003;13:164-166. 15. Johr M, Sossai R: Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg 1999;88:1051-1052. 16. Vaisman, J: Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg 2001;92:1048-1049. |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)







Post your comment