Thoraco Lumbar Paravertebral Block
|
Overview
General considerations A paravertebral block is an advanced nerve block technique. Although in principle, the technique is similar to that of the thoracic paravertebral block, its anatomy and indications are sufficiently distinct to deserve separate consideration. It is paradoxical that this technique is one of the easiest and most time efficient to perform, yet it is one of the most difficult to teach. The technique involves stereotactic needle maneuvering. A certain "mechanical" mind or sense of geometry is very helpful in mastering it. The paravertebral block is a selective block of the nerve roots at the chosen levels. The resultant anesthesia or analgesia is conceptually similar to a "unilateral" epidural anesthesia. Higher or lower levels can be chosen to accomplish a band-like segmental blockade at the desired levels. However, the paravertebral block does not result in hemodynamically significant sympathetic blockade, therefore, hypotension is not commonly seen with this block. This block is used most commonly in our practice for surgical patients undergoing inguinal herniorrhaphy. For this indication, it is important to avoid blockade of the L2 level (femoral nerve), which affects the ability to ambulate. The technique is also well suited for pain management after hip surgery (T12-L5). Regional Anesthesia Anatomy The walls of the paravertebral space in this region are formed by the parietal pleura or iliopsoas anterolaterally, vertebral body, the intervertebral disc and intervertebral foramen medially and the superior costotransverse process posteriorly (higher levels). The spinal nerves in the paravertebral space are submerged in the paravertebral adipose tissue. The paravertebral space is continuous with the epidural space medially and the contralateral paravertebral space via the prevertebral fascia. The mechanism of action of paravertebral blockade at this level includes direct penetration of the local anesthetic into the spinal nerve, and medial extension through the intervertebral foramina. Distribution of Anesthesia  Thoraco-lumbar paraverterbral block results in ipsilateral dermatomal anesthesia. The location of the resulting dermatomal distribution of anesthesia or analgesia is the function of the level blocked and the volume of local anesthetic injected. Patient Positioning  The patient is positioned in the sitting or lateral decubitus position and supported by an attendant. The back should assume kyphosis, similar to a position required for neuraxial anesthesia. The patient's feet should be rested on a stool to allow for greater comfort and a greater degree of kyphosis. This increases the distance between the adjacent transverse processes and facilitates advancement of the needle beyond the contact with the transverse process. Equipment  A standard regional anesthesia tray is prepared with the following equipment:
Landmarks  Surface Landmarks The following boney surface anatomy landmarks are helpful to identify spinal levels and to estimate the position of the transverse processes:
 Anatomic Landmarks Before attempting the block, all relevant landmarks should be outlined with a pen. These include:
Technique  Local Anesthetic Skin Infiltration After cleaning the skin with an antiseptic solution, 6-8 mL of dilute local anesthetic is infiltrated subcutaneously alongside the line where the injections will be made. The injection should be carried out slowly to avoid pain on injection and new needle reinsertions should be made through already anesthetized skin.
 Hand position The fingers of the palpating hand should straddle the paramedial line and fix the skin to avoid medial-lateral skin movement. This hand is moved in the cranial-caudal position only during the block placement. The needle is inserted perpendicular to the skin with constant attention to the depth of needle insertion and the medial-lateral needle orientation.  The entire block procedure consists of five maneuvers:
Some authors suggest using a loss of resistance technique to identify the paravertebral space. However, such a change of resistance, even when present, is very subtle and nonspecific at best. For this reason, we do not pay attention to the loss of resistance but carefully measure the skin-transverse distance and simply advance the needle 1 cm past the process. A certain "give" may be occasionally felt as the needle passes through the costotransveralis ligament, however, this is obviously not the case at the lumbar level. Proper handling of the needle is important both for accuracy and safety. Once the transverse process is contacted, the needle should be regripped so that the fingers create allow 1 cm deeper insertion. 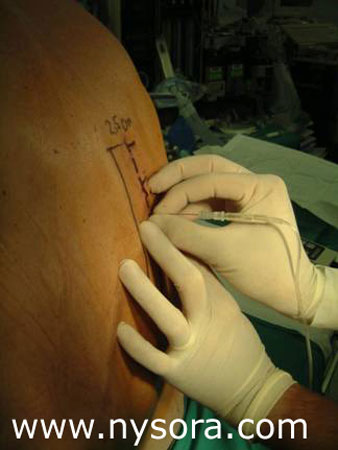
Choice of Local Anesthetic Unless lower lumbar levels (L2-5) are blocked, paravertebral blocks do not result in motor block of an extremity and do not impair the patient's ability to ambulate. In addition, relatively small volumes injected at several levels do not present a concern for local anesthetic toxicity. For these reasons, it is almost always beneficial to achieve longer acting blockade by using longer acting local anesthetic.
Block Dynamics and Perioperative Management The onset time for this block is slightly longer than in other block techniques (15-25 min). The blockade depends on anesthetic dispersion within the space to reach the individual roots at the level of the injection. The first sign of the blockade is the loss of pin-prick sensation at the dermatomal distribution of the root being blocked. The higher the concentration of the local anesthetic used, the faster the onset can be expected.
Complications and How to Avoid Them
REFERENCES: 1. Kopacz DJ., Thompson GE: Neural blockade of the Thorax and abdomen. In Cousins, M.J., and Bridenbaugh PO (eds): Neuronal Blockade in Clinical Anesthesia and Management of Pain. Philadelphia, J.B. Lippincott-Raven Publishers, 1988, pp 451-85. 2. Karmakar MK, Gin T, Ho AM: Ipsilateral thoraco-lumbar anaesthesia and paravertebral spread after low thoracic paravertebral injection. Br J Anaesth 2001; 87:312-6. 3. Karmakar MK: Paravertebral somatic nerve block for outpatient inguinal herniorrhaphy. Reg Anesth Pain Med 1999; 24:96-7. 4. Klein SM, Pietrobon R, Nielsen KC, Steele SM, Warner DS, Moylan JA, Eubanks WS, Greengrass RAL: Paravertebral somatic nerve block compared with peripheral nerve blocks for outpatient inguinal herniorrhaphy. Reg Anesth Pain Med. 2002; 27:476-80. 5. Klein SM, Greengrass RA, Weltz C, Warner DS: Paravertebral somatic nerve block for outpatient inguinal herniorrhaphy: an expanded case report of 22 patients. Reg Anesth Pain Med 1998; 23:306-10. 6. Klein SM, Pietrobon R, Nielsen KC, Steele SM, Warner DS, Moylan JA, Eubanks WS, Greengrass RA: Paravertebral somatic nerve block compared with peripheral nerve blocks for outpatient inguinal herniorrhaphy. Reg Anesth Pain Med 2002; 27:476-80. 7. Lonnqvist PA, Hildingsson U: The caudal boundary of the thoracic paravertebral space. A study in human cadavers Anaesthesia. 1992; 47:1051-2. 8. Naja Z, Ziade MF, Lonnqvist PA: Bilateral paravertebral somatic nerve block for ventral hernia repair. Eur J Anaesthesiol 2002; 19:197-202. 9. Naja Z, Lonnqvist PA. Somatic paravertebral nerve blockade. Incidence of failed block and complications. Anaesthesia 2001; 56:1184-8. 10. Pusch F, Wildling E, Klimscha W, Weinstabl C: Sonographic measurement of needle insertion depth in paravertebral blocks in women. Br J Anaesth 2002; 85: 841-3. 11. Richardson J, Vowden P, Sabanathan S: Bilateral paravertebral analgesia for major abdominal vascular surgery: <br/ >a preliminary report. Anaesthesia 1995; 50:995-8. 12. Richardson J, Sabanathan S: Thoracic paravertebral analgesia. Acta Anaesthesiol Scand 1995; 39:1005-15 13. Wheeler LJ: Peripheral nerve stimulation end-point for thoracic paravertebral block. Br J Anaesth 2001; 86:598. 14. Wyatt SS, Price RA: Complications of paravertebral block. Br J Anaesth 2000; 84:424. 15. Wassef MR, Randazzo T, Ward W: The paravertebral nerve root block for inguinal herniorrhaphy--a comparison with the field block approach. Reg Anesth Pain Med 1998; 23:451-6. 16. Wood GJ, Lloyd JW, Bullingham RE, Britton BJ, Finch DR. Postoperative analgesia for day-case herniorrhaphy patients. |
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)


















Post your comment