Supraclavicular Brachial Plexus Block
|
Figure 1: Insertion of the needle in the supraclavicular brachial plexus block. The needle is inserted lateral to the insertion of the clavicular head of the sternocleidomastoid muscle. Essentials
Supraclavicular Block General Considerations The supraclavicular approach to the brachial plexus characteristically is associated with a rapid onset of anesthesia and a high success rate. The first percutaneous supraclavicular block was performed by Kulenkampff in Germany in 1911, reportedly on himself. A few months after, Hirschel described a method of brachial plexus with an axillary approach. In 1928, Kulenkampff and Persky published their experiences with a thousand blocks without apparent major complications. Kulenkampff's technique required the patient to be in the sitting position. The needle insertion was above the midpoint of the clavicle in the direction of the spinous process of T2 or T3. Unfortunately, this medial orientation of the needle was associated with a risk of pneumothorax, which eventually became the reason for the supraclavicular block to fall into disfavor in many centers. Since then, many modifications to the original technique were proposed to decrease the risk for pneumothorax. The technique described in this chapter takes into account the location of the dome of the pleura to reduce the risk for pneumothorax. The advantages of a supraclavicular technique over other brachial plexus block approaches are its rapid onset and complete and predictable anesthesia for entire upper extremity and particularly, hand surgery. The introduction of ultrasound guidance to regional anesthesia in the last decade has resulted in significant renewed interest in the clinical application of the supraclavicular block, as well as a greater understanding of its mechanics. Functional Anatomy The supraclavicular block is often called the "spinal anesthesia of the upper extremity" because of its ubiquitous application for upper extremity surgery. The reasons for its high success rate are in its anatomic characteristics. The block is performed at the level of the distal trunks and origin of the divisions, where the brachial plexus is confined to its smallest surface area (Figure 2A). The three trunks carry the entire sensory, motor, and sympathetic innervation of the upper extremity, with the exception of the uppermost part of the medial side of the arm (T2). The densely packed divisions, in contrast, carry a similar amount of innervation in a slightly larger surface area, but there is a larger surface of absorption. Another important anatomic feature of the supraclavicular block is the presence of the subclavian artery in front of the lower trunk and its divisions (Figure 2B). To increase the chance of blocking C8-T1 dermatomes it may be eneficial to insert the needle in the proximity of the lower trunk and make it the focal point of injection. The sternocleidomastoid muscle inserts on the medial third of the clavicle, the trapezius inserts on the lateral third, and the neurovascular bundle passes underneath the middle third, which includes the midpoint of the clavicle. During a supraclavicular block, the pleura potentially can be breached either at the pleural dome (more likely) or through the first intercostal space. A practical knowledge of the anatomical position of the pleura is important to decrease the risk of pneumothorax. The pleural dome is contained within the concavity of the first rib. Because the first rib crosses under the junction between the medial and middle thirds of the clavicle (Figure 3), its path coincides with the insertion of the sternocleidomastoid muscle, which inserts on the medial third of the clavicle. Therefore, the lateral insertion of the sternocleidomastoid muscle on the clavicle can be used as a landmark for the location of the first rib and of the lateral edge of the dome of the pleura. The first intercostal space, in contrast, is for the most part infraclavicular, and consequently it should not be reached during a supraclavicular block.
Distribution of Blockade The supraclavicular block results in anesthesia of dermatomes C5 through T1, making it suitable for anesthesia or analgesia of the entire upper extremity distal to the shoulder, including the upper arm and elbow as well as the forearm, wrist, and hand.
Figure 3: Radiocontrast image of the mixture of local anesthetic and radiopaque solution injected in the supraclavicular brachial plexus. The contrast is shown descending from the lower aspect of the clavicle toward the axillary fossa. Equipment
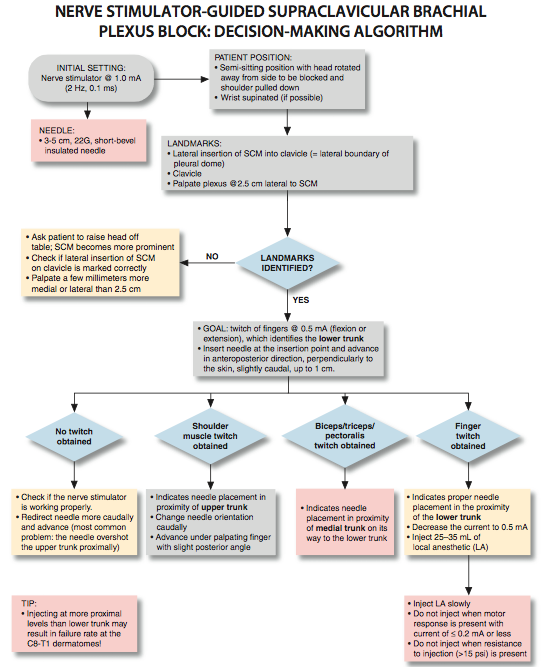
Landmarks and Patient Positioning The patient is placed in a semi-sitting position with the head rotated away from the site to be blocked and the shoulder pulled down. The arm rests comfortably on the side while the wrist, if possible, is supinated (Figure 4). The main landmarks for this block are the lateral insertion of the sternocleidomastoid muscle onto the clavicle and the clavicle itself. Light premedication (e.g., midazolam 1 mg and fentanyl 50 µg IV repeated as necessary) is beneficial for patient comfort.
Maneuvers to Facilitate Landmark Identification To facilitate the recognition of the sternocleidomastoid muscle, the patient can be asked to elevate the head off the pillow, as shown in Figure 5. Once the sternocleidomastoid is identified, a mark is placed on the clavicle at its lateral insertion, as shown in Figure 6.
Technique After identifying the lateral insertion of the sternocleidomastoid muscle on the clavicle, the operator locates the plexus by palpation, which in adults is found at about 2.5 cm lateral to the sternocleidomastoid. Once the plexus is found, the point of needle insertion is located immediately cephalad to the palpating finger, as shown in Figure 7. The nerve stimulator is connected to the stimulating needle and set to deliver a 0.8 to 1.0 mA current at 1 Hz frequency and 0.1 ms of pulse duration.The needle is inserted first in an anteroposterior direction, almost perpendicularly to the skin with a slight caudal orientation, as shown in Figure 1.
The needle is slowly advanced until the upper trunk is identified by a muscle twitch of the shoulder muscles or up to 1 cm, if there is no response. At this point, the orientation of the needle is changed to advance it now caudally under the palpating finger, with a slight posterior angle, as shown in Figure 8. This strategy directs the needle from the vicinity of the upper trunk (shoulder twitch) to the front of the medial trunk (biceps, triceps, pectoralis twitch) on its way to the lower trunk (fingers twitch).
Once the elicited motor response of the fingers is obtained at 0.5 mA, the injection is carried out after gentle aspiration. Injecting in the proximity of the lower trunk (motor response of the fingers) is the most important factor in accomplishing a successful supraclavicular brachial plexus block. For surgical anesthesia, we commonly select 25 to 35 mL of 1.5% mepivacaine with 1:300,000 epinephrine, for a 3- to 4-hour duration of anesthesia and a variable, but usually short, duration of analgesia. We use a similar volume of 3% 2-chloroprocaine for a duration of 60 to 90 minutes of anesthesia for shorter cases. For analgesia, 20 mL of 0.2% ropivacaine with 1:300,000 epinephrine as an intravascular marker can be selected. Troubleshooting Maneuvers

Figure 8: Insertion of the needle for the supraclavicular brachial plexus block.
Contraindications Supraclavicular block should not be done bilaterally because of the potential risk of respiratory compromise secondary to pneumothorax or phrenic nerve block. Although this recommendation seems logical, there is no evidence in the literature that bilateral supraclavicular block is actually contraindicated. Although phrenic nerve palsy may occur after approximately 50% of supraclavicular blocks, very few patients are symptomatic. Regardless, performing the block in patients with chronic respiratory problems, especially those using accessory respiratory muscles, is a decision that must be made on a case-by-case basis because any choice of anesthesia, including general anesthesia, will have important implications in these patients.
|
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)
![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)
























Post your comment