Cutaneous Nerve blocks of the Upper Extremity
|
A
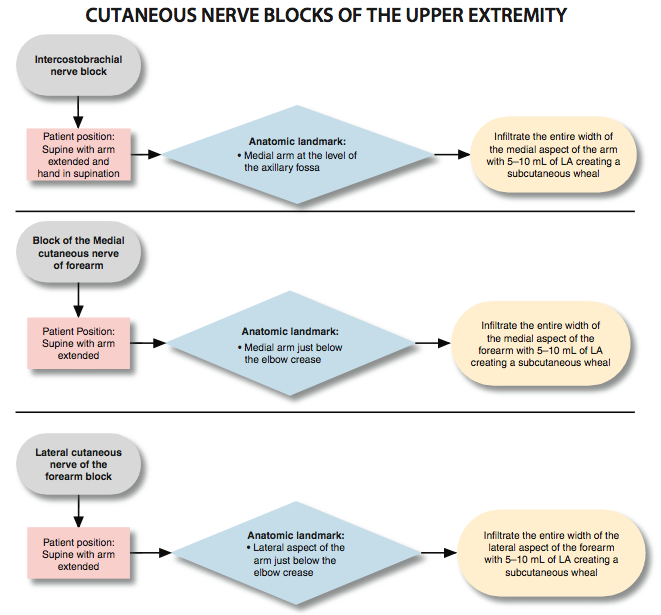
Figure 1: Techniques to block the cutaneous nerves of the upper extremity. Essentials
General Considerations Cutaneous nerve blocks of the upper extremity are used mainly as a supplement to brachial plexus blocks. These blocks are simple to learn and perform. They are essentially devoid of complications and can be useful as complements to major conduction blocks of the upper extremity. Their judicious use can be used for superficial surgery or to help salvage an incomplete brachial plexus block. The techniques discussed in this chapter focus primarily on the blocks that are most useful clinically: blocks of the intercostobrachial nerve and the medial and lateral cutaneous nerves of the forearm, Figure 1. Functional Anatomy Cutaneous nerve blockade is achieved by the injection of local anesthetic into the subcutaneous layers above the muscle fascia. The subcutaneous tissue contains a variable amount of fat, superficial nerves, and vessels. Deeper, there is a tough membranous layer, the deep fascia of the upper extremity, which encloses the muscles of the arm and fore- arm. Numerous superficial nerves and vessels penetrate the deep fascia. The cutaneous innervation of the upper extremity originates from the superficial cervical plexus, the brachial plexus, and the intercostal nerves (Table 1; Figure 2A and B). Familiarity with their relevant anatomy is important to avoid sparing of cutaneous anesthesia during a nerve block procedure. For example, a brachial plexus block does not anesthetize the intercostobrachial nerve, a branch of T2 that is responsible for sensation of the skin of the proximal medial arm. Failure to supplement this may result in discomfort at skin incision during upper extremity surgery. Similarly, a single-injection axillary brachial plexus block typically does not cover the musculocutaneous nerve (and its terminal branch, the lateral cutaneous nerve of the forearm). A cutaneous block of this terminal branch is a more distal alternative to a musculocutaneous nerve block that provides the same sensory anesthesia. Intercostobrachial Nerve Block Anatomy The intercostobrachial nerve is the lateral cutaneous branch of the ventral primary ramus of T2. It provides innervation to the skin of the axilla and the medial aspect of the proximal arm. The intercostobrachial nerve communicates with the medial cutaneous nerve of the arm, which is a branch of the brachial plexus (Figure 3). Both nerves are anesthetized by subcutaneous infiltration of the skin of the medial aspect of the arm. Indications Blocks of these nerves are typically combined with brachial plexus block to achieve more complete anesthesia of the upper arm. Technique A 1.5-in, 25-gauge needle is inserted at the level of the axillary fossa (Figure 4A). The entire width of the medial aspect of the arm is infiltrated with local anesthetic to raise a subcutaneous wheal of anesthesia. Table 1: Origin of the Cutaneous Nerves of the Upper Extremity 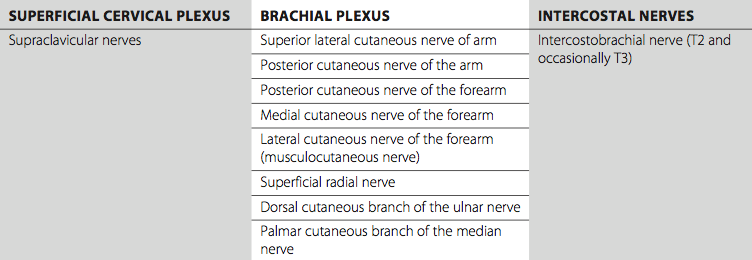
Figure 2: (A) Cutaneous innervation of the upper extremity (front).
Figure 2: (B) Cutaneous innervation of the upper extremity (back).
Figure 3: Anatomy of the terminal nerves of the upper extremity at the level of the axillary fossa. (1) axillary artery. (2) intercostobrachial nerve. (3) ulnar nerve. (4) median nerve. (5) radial nerve. (6) musculocutaneous nerve.
A
Figure 4. (A) Block of the intercostobrachial nerve. (B) Block of the medial cutaneous nerve of the forearm. (C) Block of the lateral cutaneous nerve of the forearm. Medial Cutaneous Nerve of the Forearm Block  Figure 5: Medial cutaneous nerve of the arm (arrow). Anatomy The medial cutaneous nerve of the forearm originates within the medial cord. This nerve supplies branches to the skin of the medial side of the forearm (Figure 5). Indications The medial antebrachial cutaneous nerve is blocked by infiltration of local anesthetic into the subcutaneous tissue on the anteromedial and dorsomedial surfaces of the forearm just below the elbow crease. Along with blockade of the lateral antebrachial cutaneous nerve, this block is appropriate for the insertion of an arteriovenous graft on the forearm or other superficial procedures on the volar surface of the forearm. Technique A 1.5-in, 25-gauge needle is used to infiltrate local anesthetic subcutaneously over the entire medial aspect of the arm just below the elbow crease (Figure 4B).
Figure 6. (1) Lateral cutaneous nerve of the (right) forearm, (2) Biceps muscle, (3) Brachioradialis muscle. Lateral Cutaneous Nerve of the Forearm Block Anatomy Table 2: Complications of Cutaneous Blocks and Preventive Techniques 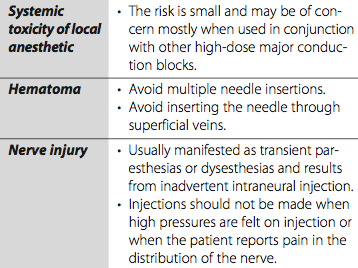 Indications Blockade of the lateral cutaneous and medial cutaneous nerves of the forearm results in anesthesia of the anterior and lateral surfaces of the forearm. This block is suitable for the insertion of arteriovenous grafts or other superficial procedures on the volar aspect of the forearm. It is also useful for supplementing an axillary brachial plexus block in which a separate musculocutaneous nerve block was not performed or failed. Technique The nerve can be blocked at the level of the arm (musculocutaneous block; see "Axillary Block" for a description) or when it emerges at the elbow level. To block the lateral cutaneous nerve of the forearm at the level of the elbow, a 1.5-in, 25-gauge needle is used to infiltrate local anesthetic subcutaneously over the entire lateral aspect of the arm just below the elbow crease (Figure 4C). Complications and How to Avoid Them Complications from cutaneous nerve blocks are few; they are discussed in Table 2
|
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)






















Post your comment