July 2014 - Newsletter
|
NYSORA - Affiliated 12 months Fellowship Training in Regional Anesthesia in Belgium  NYSORA announces a unique educational opportunity in Belgium for a qualified candidate: 12 months NYSORA Fellowship - The New York School of Regional Anesthesia- affiliated Fellowship in Regional Anesthesia leading to the NYSORA Diploma upon successful completion. The fellowship position is starting Nov 1, 2024 through October 30th 2015 in affiliation with the Department of Anesthesiology at ZOL – Ziekenhuis Oost-Limburg, Belgium in a new ultra-modern facility and with one of the most progressive orthopedic surgery centers in Europe. The fellowship will focus on wide range of clinical regional anesthesia, ultrasound anatomy, with opportunity to participate in NYSORA lead research, writing camps, and teaching at international NYSORA-sponsored workshops and symposia http://www.nysora.com/.
|
||
 Ana Lopez and John Laur instructing workshop sessions at NYSORA In this issue: |
 NYSORA September Symposium |
 NYSORA Middle East 2015 The Symposium will focus on comprehensive review of new developments in anesthesiology, pain and perioperative medicine. To accomplish its educational mission in the Middle East, NYSORA will offer a multitude of highly versatile and focused workshops. |
|
Quick Reference Guide for Regional Anesthesia in the Anticoagulated Patient 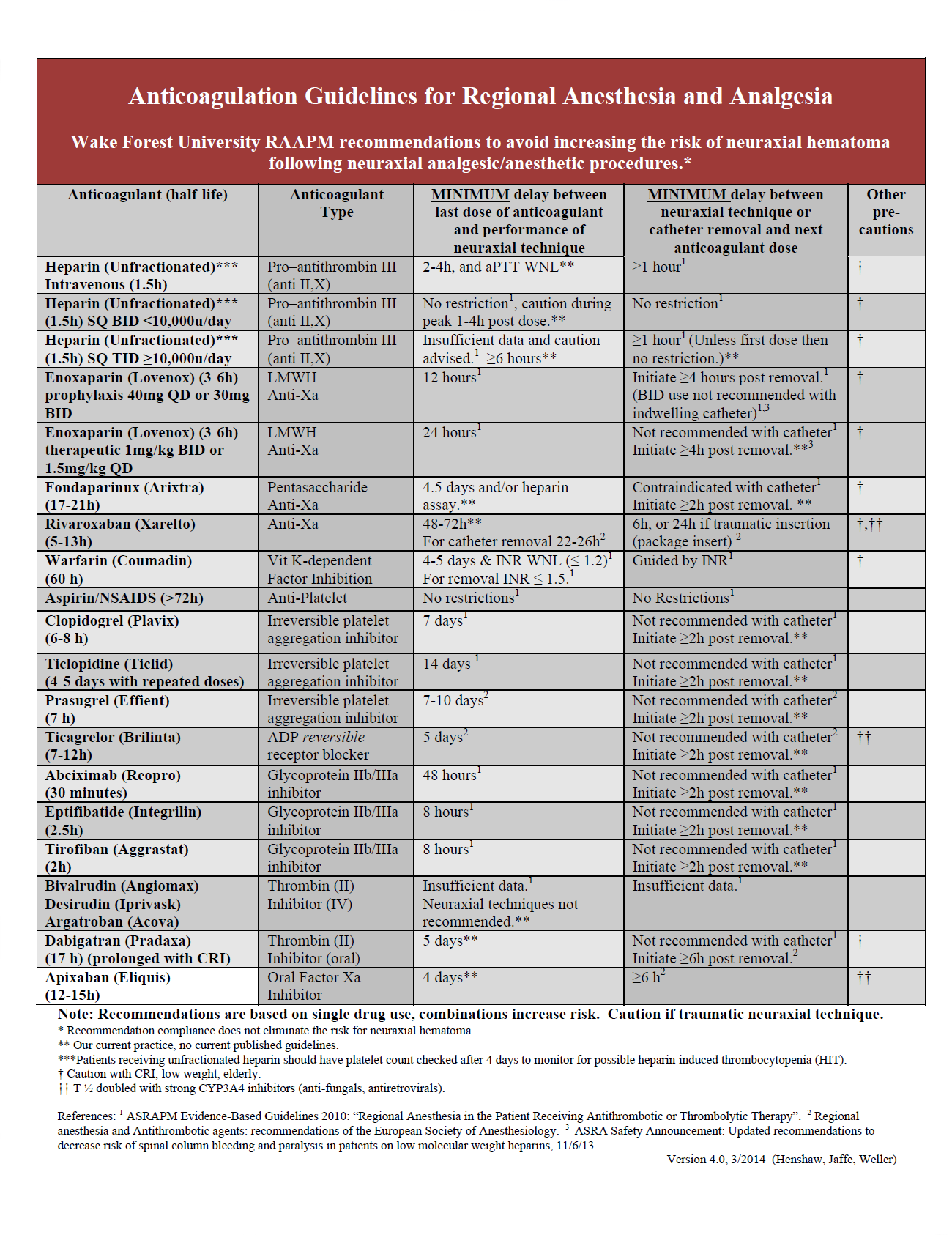 The number of anticoagulant medications being used in clinical practice has increased dramatically over the last few years as several new drugs have received approval from the United States Food and Drug Administration (FDA) for a variety of antithrombotic indications. Not only have these newer medications been quickly added to hospital formularies, they have also been increasingly prescribed in the outpatient setting for a variety of reasons: direct-to-consumer advertising, attractive route and dosing schedules, and obviation of required routine laboratory evaluation to assess therapeutic efficacy. Consequently, anesthesia providers are regularly encountering patients who take these medications in the perioperative setting. This has challenged clinicians to remain knowledgeable about the pharmacokinetics of these drugs and their associated risks when regional anesthesia or analgesia techniques are considered. Unfortunately, current published anticoagulation guidelines for regional anesthesia and analgesia have not yet addressed many of these newer medications and, when recommendations are available, they often differ depending on the resource. Not only does this increase the complexity of clinical decision-making, it may also increase the risks for the patient given the likelihood that their provider may be unfamiliar with these new antithrombotic therapies and perform a regional anesthetic, and more specifically neuraxial procedures or deep plexus blocks, when the likelihood of bleeding complications is increased. When faced with a patient who has recently taken an anticoagulant medication for which published guidelines are lacking, clinicians must independently decide, based on their understanding of pharmacokinetics and pharmacodynamics, how long this medication should be stopped before preceding with certain regional anesthesia and analgesia procedures without an unacceptable increase in the risks of bleeding complications. Additionally, following the performance of a neuraxial or deep plexus block procedure, including the removal of an indwelling catheter, clinicians must determine how long of a delay is required until the next dose of this medication can be administered. At our institution, clinicians were often challenged to accurately and quickly make decisions when confronted with similar clinical scenarios. Because the potential complications associated with the performance of neuraxial or deep plexus block procedures can be devastating when residual anticoagulant medication effects exist, these types of procedures were often avoided due to a perceived increased risk of complications, even in patients with significant comorbidities in whom regional anesthesia may have been preferred. In 2012, with the goal of simplifying the process by which anesthesiologists at our institution determine whether a patient being treated with anticoagulant medications was at an unacceptably increased risk of bleeding complications following the performance of a regional technique, a guideline reference chart was created by consolidating the available published guidelines from the American Society of Regional Anesthesia (ASRA)1 and the European Society of Anesthesiology (ESA)2. For anticoagulant agents that lacked formal published guidelines pharmacokinetic data (drug half-life) was used to estimate the recommended time interval between the last dose of a drug and the performance of a neuraxial or deep plexus procedure; it was generally assumed that 5 half-lives were necessary to achieve near complete resolution of drug effect. Longer durations were recommended if the clearance of a drug might be affected by renal insufficiency. Since inception the reference chart has undergone several updates either as new recommendations were released or as new anticoagulant medications received FDA approval. It was first presented outside of our institution at a problem-based learning discussion during the annual NYSORA symposium in 2012. The most recent version of the reference chart (Figure 1) includes the recent recommendation from both ASRA and the FDA to allow at least four hours between the performance of a neuraxial procedure (such as epidural catheter removal) and the administration of the next dose of enoxaparin.3 The ubiquitous availability of this anticoagulation reference chart has allowed clinicians at our institution to more quickly and accurately determine if a patient is at an unacceptably increased risk of bleeding following a regional anesthetic procedure based on the currently available guidelines and/or pharmacologic data. It has become routinely used across the four hospitals within our health care system, not just by anesthesia providers, but also by clinicians in multiple specialties since the universal pre-procedure checklist at our institution now includes a step to review and consider the patient's current coagulation status before any invasive procedure. By consolidating this information into one easy to reference location we believe we have improved the efficiency of our operating rooms as well as the safety of our patients both within and beyond the walls of our operating rooms. References: Daryl Henshaw, MD  Robert S. Weller, Daryl Henshaw and J. Douglas Jaffe Wake Forest School of Medicine Department of Anesthesiology Section of Regional Anesthesia and Acute Pain Management Winston Salem, NC 27157 |
|
NYSORA subspecialty focus workshop highlight - Pediatric Regional Anesthesia
In an effort to meet the demands of our delegates for basic and advanced workshops in a variety of specialized topics, this year the first Pediatric Regional Workshop will be held at NYSORA 2014. This workshop will focus on basic ultrasound based regional anesthesia techniques designed for novices and intermediate skill level practitioners who desire to learn more about the blocks provided every day in a busy pediatric practice. Delegates will become familiar with basic principles of ultrasonography and needle maneuvering, applied anatomy, and will scan pediatric models. Colleagues who are more advanced will be grouped together to allow for more rapid progression of topics and more advanced learning. Course Instructors: Karen Boretsky MD and Steven Orebaugh MD  |
||
|
Featured Educational Video - Ultrasound-Guided Interscalene Brachial Plexus Block |
 |

![[advertisement] concertmedical](../../files/bk-nysora-ad.jpg)













 Educational Material Download
Educational Material Download![[advertisement] gehealthcare](../../files/banners/banner1_250x600/GEtouch(250X600).gif)
Post your comment