Sciatic Nerve Block: Anterior / Transgluteal / Subgluteal Approach
Figure 1: (A) Needle insertion to block the sciatic nerve using an anterior approach. Note that a curved (phased array) lower frequency transducer is used either in-plane (shown) or out-of-plane needle insertion can be used. (B) Transgluteal approach to sciatic block; patient position, transducer (curved) placement and needle insertion. Essentials
PART 1: ANTERIOR APPROACH  Figure 1-2: Cross-sectional anatomy of the sciatic nerve (ScN). Shown are femoral artery (FA), adductor longus muscle (ALM), pectineus muscle, adductor magnus muscle (AMM), adductor brevis muscle (ABM), gracilis muscle (GsM), and the femur. The sciatic nerve is seen posterior to the AMM.
Figure 1-3: Ultrasound anatomy of the sciatic nerve. From superficial to deep; femoral artery (FA) and femur laterally, adductor magnus muscle (AMM) and sciatic nerve (ScN) laterally. The sciatic nerve is typically located at a depth of 6 to 8cm. General Considerations The anterior approach to sciatic block can be useful in patients who cannot be positioned in the lateral position due to pain, trauma, presence of external fixation devices interfering with positioning, and other issues. It also may be well-suited to patients who require postoperative blocks for analgesia following a total knee arthroplasty. Ultrasonography adds the benefit of no requirement for the palpation of a femoral pulse or the use of geometry for identification of the skin puncture point. In addition, using the ultrasound-guided approach should reduce the risk of puncture of the femoral artery as compared with the landmark-based approach. The actual scanning and needle insertion are performed on the anteromedial aspect of the proximal thigh, rather than the anterior surface, and may require a slight abduction and external rotation of the thigh. This block is not well suited to insertion of catheters because a large needle must traverse several muscles (causing pain and possibly hematomas), an awkward catheter location (medial thigh), and catheter insertion at approximately perpendicular angle to the sciatic nerve is difficult. Ultrasound Anatomy The sciatic nerve is imaged approximately at the level of the minor trochanter. At this location, a curved transducer placed over the anteromedial aspect of the thigh will reveal the musculature of all three fascial compartments of the thigh: anterior, medial, and posterior (Figures 1-2 and 1-3). Beneath the superficial sartorius muscle is the femoral artery, and deep and medial to this vessel is the profunda femoris artery. Both of these can be identified with color Doppler ultrasound for orientation. The femur is easily seen as a hyperechoic rim with the corresponding shadow beneath the vastus intermedius. Medial to the femur is the body of the adductor magnus muscle, separated by the fascial plane(s) of the hamstrings muscles. The sciatic nerve is visualized as a hyperechoic, slightly flattened oval structure sandwiched between these two muscle planes. The nerve is typically visualized at a depth of 6 to 8 cm (Figure 1-3).  Figure 1-4: Transducer position to visualize the sciatic nerve through the anterior approach. Distribution of Blockade Sciatic nerve block results in anesthesia of the posterior aspect of the knee, hamstrings muscles, and entire lower limb below the knee, both motor and sensory, with the exception of skin on the medial leg and foot (saphenous nerve). The skin of the posterior aspect of the thigh is supplied by the posterior cutaneous nerve of the thigh, which has its origin from the sciatic nerve more proximal than the anterior approach. It is, therefore, not blocked by the anterior approach. Practically, however, the lack of anesthesia in its distribution is of little clinical consequence. Equipment Equipment needed is as follows:
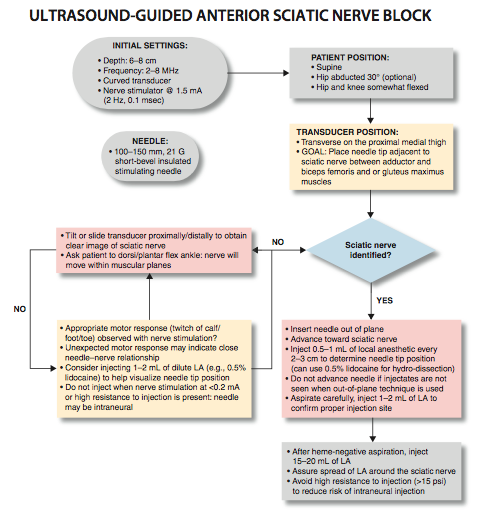
Landmarks and Patient Positioning Anterior approach to sciatic nerve block is performed with the patient in the supine position. The hip is abducted to facilitate transducer and needle placement (Figure 1-4 and 1-5). When feasible, the hip and knee should be somewhat flexed to facilitate exposure. If nerve stimulation is to be used at the same time (recommended), exposure of the calf and foot are required to observe motor responses. In either case, it is useful to expose the entire thigh to appreciate the distance from the groin to knee.
Technique With the patient in the proper position, the skin is disinfected and the transducer positioned so as to identify the sciatic nerve. If the nerve is not immediately apparent, sliding and tilting the transducer proximally or distally can be useful to improve the contrast and bring the nerve 'out' of the background from the musculature. Finally, if the patient is able to dorsiflex and/or plantar flex the ankle, this maneuver often causes the nerve to rotate or otherwise move within the muscular planes, facilitating identification. Once identified, the needle is inserted in-plane or out of plane (more common in our program) from the medial aspect of the thigh and advanced toward the sciatic nerve (Figure 1-5). If nerve stimulation is used (1.0 mA, 0.1 msec), the contact of the needle tip with the sciatic nerve is usually associated with a motor response of the calf or foot. Once the needle tip is deemed to be in the proper position, 1 to 2 mL of local anesthetic is injected to confirm the adequate distribution of injectate. Such injection helps delineate the sciatic nerve within its intramuscular tunnel, but it may displace the sciatic nerve away from the needle. Improper spread of the local anesthetic or nerve displacement may require an additional advancement of the needle. When injection of the local anesthetic does not appear to result in a spread around the sciatic nerve, additional needle repositions and injections are necessary.
In an adult patient, 15 to 20 mL of local anesthetic is usually adequate for successful blockade (Figure 1-6). Although a single injection of such volume of local anesthetic suffices, it may be beneficial to inject two to three smaller aliquots at different locations to assure the spread of the local anesthetic solution around the sciatic nerve.
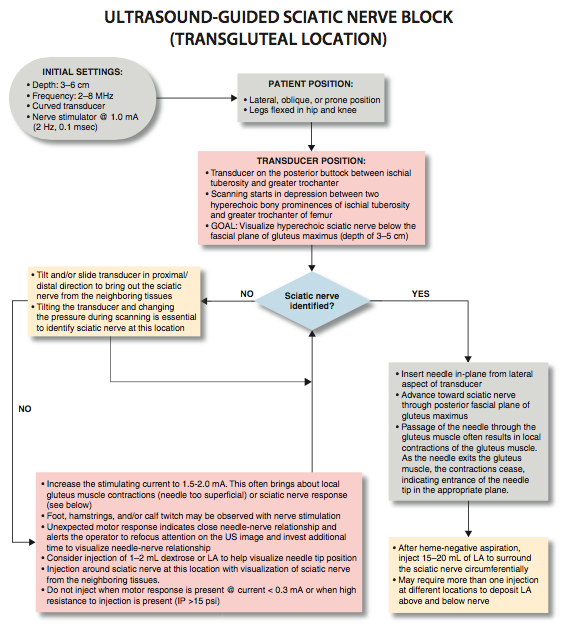
PART 2: TRANSGLUTEAL AND SUBGLUTEAL APPROACH  Figure 2-1: Transsectional anatomy of the sciatic nerve at the transgluteal level. Sciatic nerve (ScN) is seen between the greater trochanter of the femur and the ischium tuberosity, just below the gluteus maximus (GMM) muscle.
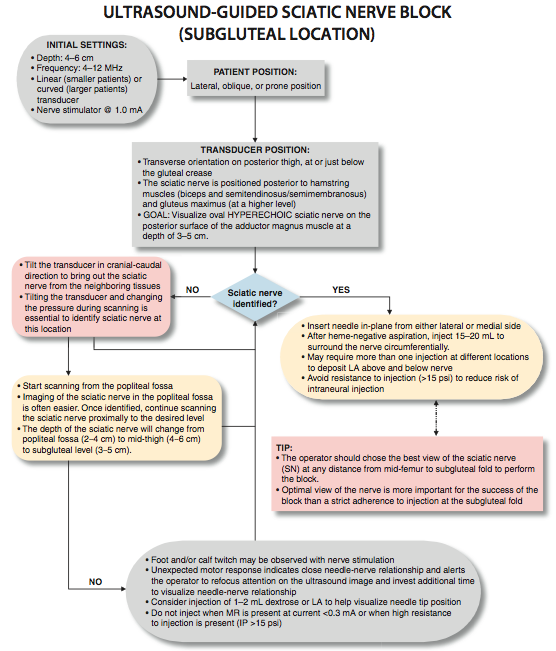
FIgure 2-2: An ultrasound image demonstrating the sonoanatomy of the sciatic nerve (ScN). The ScN often assumes an ovoid or triangular shape and it is positioned underneath the gluteus muscle (GMM) between the ischium tuberosity (IT) and femur. General Considerations The use of ultrasonographic guidance greatly expanded the options that practitioners have for accomplishing the block of the sciatic nerve because the nerve can be imaged at several convenient levels. With the transgluteal approach, the needle is inserted just distal deep to the gluteus maximus muscle to reach the sciatic nerve. The sciatic nerve at the gluteal crease is readily identified in a predictable anatomic arrangement, between two osseous landmarks (ischial tuberosity and the greater trochanter) and beneath a well-defined muscle plane. The use of ultrasound visualization decreases the need for the geometry and measurements that are required for the classic landmark-based approaches. With the subgluteal approach, the nerve simply reached a few centimeters distally, just below the level of the subgluteal crease where imaging is not interfered by the bones. The preference of one approach over the other is made based on the patient's anatomic characteristics and personal preference. Ultrasound Anatomy At this transgluteal level, the sciatic nerve is visualized in the short axis between the two hyperechoic bony prominences of the ischial tuberosity and the greater trochanter of the femur (Figure 2-1 and 2-2). The gluteus maximus muscle is seen as the most superficial muscular layer bridging the two osseous structures, typically several centimeters thick. The sciatic nerve is located immediately deep to the gluteus muscles, superficial to the quadratus femoris muscle. Often, it is slightly closer to the ischial tuberosity (medial) aspect than the greater trochanter (lateral). At this location in the thigh, it is seen as an oval or roughly triangular hyperechoic structure. At the subgluteal level, however, the sciatic nerve is positioned deep to the long head of the biceps muscle and the posterior surface of the adductor magnus.
Figure 2-3: Patient position and transducer application for subgluteal appraoch to sciatic block
Figure 2-4: Transgluteal approach to sciatic block; patient position, transducer (curved) placement and needle insertion. Distribution of Blockade Sciatic nerve block results in anesthesia of the entire lower limb below the knee, both motor and sensory blockade, with the exception of a variable strip of skin on the medial leg and foot, which is the territory of the saphenous nerve, a branch of the femoral nerve. In addition, both the transgluteal and subgluteal approaches provide motor blockade of the hamstring muscles. The skin of the posterior aspect of the thigh however, is supplied by the posterior cutaneous nerve of the thigh, which has its origin from the sciatic nerve more proximal than the subgluteal approach. It is, therefore, unreliably anesthetized with subgluteal block; however, it is of relatively little clinical importance.  Figure 2-5: Sciatic nerve (yellow arrows) as seen in the subgluteal position (linear transducer), needle path (white arrows) and local anesthetic (turquoise arrows) in the intramuscular tunnel surrounding the sciatic nerve. Equipment Equipment needed is as follows:
Landmarks and Patient Positioning Any patient position that allows for comfortable placement of the ultrasound transducer and needle advancement is appropriate. Typically for either the transgluteal or subgluteal block, this involves placing the patient in a position between the lateral decubitus and prone position (Figures 2-3 and 2-4). The legs are flexed in the hip and knee. When nerve stimulation is used simultaneously (suggested), exposure of the hamstrings, calf, and foot is required to detect and interpret motor responses. The round osseous prominences of the greater trochanter and ischial tuberosity are palpated and, if desired, marked with a skin marker. Scanning is begun in the depression between the two bones.
Technique The description of the technique in this chapter will focus primarily on the transgluteal approach. However, since the subgluteal approach is performed just a few centimeters more distal and it is technically easier, the reader can easily perform either approach by using general guidelines provided and referring to Figure 2-3, Figure 2-4, and algorithms at the end of the chapter. With the patient in the described position, the skin is disinfected and the transducer is positioned so as to identify the sciatic nerve (Figure 2-4). If the nerve is not immediately apparent, tilting the transducer proximally or distally can help improve the contrast and bring the nerve “out” of the background of the musculature. Often, the nerve is much better imaged after the injection of local anesthetic (Figure 2-5). Alternatively, sliding the transducer slightly proximally or distally can improve the quality of the image and allow for better visualization. Once identified, the needle is inserted in-plane, typically from the lateral aspect of the transducer and advanced toward the sciatic nerve. If nerve stimulation is used (1.0 mA, 0.1 msec), the passage of the needle through the anterior fascial plane of the gluteus muscles often is associated with a motor response of the calf or foot. Once the needle tip is positioned adjacent to the nerve (Figure 2-6A) and after careful aspiration to rule out an intravascular needle placement, 1 to 2 mL of local anesthetic is injected to document the proper injection site. Such injection often displaces the sciatic nerve away from the needle; therefore, an additional advancement of the needle 1 to 2 mm toward the nerve may be necessary to ensure the proper spread of the local anesthetic. When injection of the local anesthetic does not appear to result in a spread around the sciatic nerve, additional needle repositions and injections may be necessary. Assuring the absence of high resistance to injection is of utmost importance because the needle tip is difficult to visualize on ultrasound due to the steep angle and depth of the needle placement.
Figure 2-6: (A) Ultrasound image demonstrating the simulated needle path to reach the sciatic nerve (ScN) using an in-plane technique in transgluteal approach. The simulated needle (1) is shown transversing the gluteus muscle with its tip positioned at the lateral aspect of the sciatic nerve. (B) Needle path and distribution of local anesthetic (blue shaded area) to block the ScN through the transgluteal approach. In an adult patient, 15 to 20 mL of local anesthetic is usually adequate for successful blockade of sciatic nerve (Figure 2-6). Although a single injection of such volumes of local anesthetic suffices, it may be beneficial to inject two to three smaller aliquots at different locations to ensure the spread of the local anesthetic solution around the sciatic nerve.
Continuous Ultrasound-Guided Subgluteal Sciatic Block The goal of the continuous sciatic block is similar to the non-ultrasound-based techniques: to place the catheter in the vicinity of the sciatic nerve between the gluteus maximus and quadratus femoris muscles. The procedure consists of three phases: needle placement, catheter advancement, and securing the catheter. For the first two phases of the procedure, ultrasound visualization can be used to ensure accuracy in most patients. The needle typically is inserted in-plane from the lateral to medial direction and underneath the fascia to enter the subgluteal space. Advancement of the needle until the tip is adjacent to the nerve and deep to the gluteus maximus fascia should ensure appropriate catheter location. Proper placement of the needle also can be confirmed by obtaining a motor response of the calf or foot at which point, 4 to 5 mL of local anesthetic is injected. This small dose of local anesthetic serves to ensure adequate distribution of the local anesthetic as well as to make the advancement of the catheter easier. This first phase of the procedure does not significantly differ from the single-injection technique. The second phase of the procedure involves maintaining the needle in the proper position and inserting the catheter 3 to 5 cm beyond the needle tip into the subgluteal space in the vicinity of the sciatic nerve. Insertion of the catheter requires an assistant when it is done under ultrasound guidance. Alternatively, the catheter can be inserted using a longitudinal view. With this approach, after successful imaging of the sciatic nerve in the cross-sectional view, the transducer is rotated 90 degrees so that the sciatic nerve is visualized in the longitudinal view. However, this approach requires significantly greater ultrasound imaging skills. The catheter is secured by either taping it to the skin or tunneling. A common infusion strategy includes ropivacaine 0.2% at 5 mL/minute with a patient-controlled bolus of 5 mL/hour.
|
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)


























Post your comment