Interscalene Brachial Plexus Block
|
Figure 1: Needle insertion for interscalene brachial plexus block. The needle is inserted between palpating fingers that are positioned in the scalene groove (between anterior and middle scalene muscles). 1 = sternal head of the sternocleidomastoid muscle. 2 = clavicular head of the sternocleidomastoid muscle. Essentials
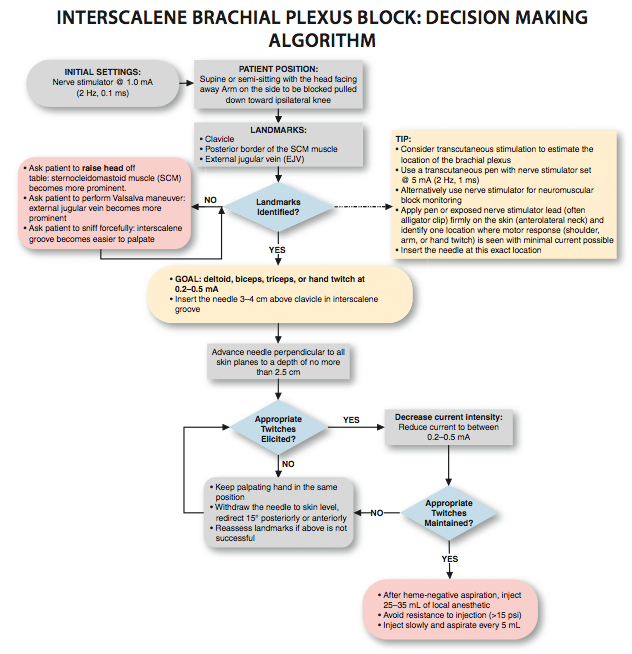
General Considerations An interscalene block relies on the spread of a relatively large volume of local anesthetic within the interscalene groove to accomplish blockade of the brachial plexus. In our practice, we almost always use a low interscalene block technique, which consists of inserting the needle more caudally than in the commonly described procedure performed at the level of the cricoid cartilage. Our reasoning is that at the lower neck, the interscalene groove is more shallow and easier to identify, and the distribution of anesthesia is also adequate for elbow and forearm surgery. In addition, the needle insertion is more lateral, which makes puncture of the carotid artery less likely and performance of the block easier to master by trainees. Low approach to interscalene block is used in shoulder, arm, and forearm surgery. In our practice, the most common indications for this procedure are shoulder and humerus surgery and the insertion of an arteriovenous graft for hemodialysis. Functional Anatomy 
Figure 2: Anatomy of the brachial plexus. The sternocleidomastoid muscle is removed and the brachial plexus (1) is seen emerging between the scalene muscles. (2) internal jugular vein. (3) carotid artery. (4) subclavian artery. (5) Retracted pectoralis muscle. (6) medial and lateral pectoral nerves. The number "1" also indicates the approximate level at which the block is performed where the roots of the muscles are emerging between the scalene muscles. The brachial plexus supplies innervation to the upper limb and consists of a branching network of nerves derived from the anterior rami of the lower four cervical and the first thoracic spinal nerves. Starting from their origin and descending distally, the components of the plexus are named roots, trunks, divisions, cords, and, finally, terminal branches. The five roots of the cervical and the first thoracic spinal nerves (anterior rami) give rise to three trunks (superior, middle, and inferior) that emerge between the medial and anterior scalene muscles to lie on the floor of the posterior triangle of the neck (Figure 2). The roots of the plexus lie deep to the prevertebral fascia, whereas the trunks are covered by its lateral extension, the axillary sheath. Each trunk divides into an anterior and a posterior division behind the clavicle, at the apex of the axilla (Figure 3). The divisions combine to produce the three cords, which are named lateral, median, and posterior according to their relationship to the axillary artery. From this point on, individual nerves are formed as these neuronal elements descend distally (Figure 3 and Table 1) 
Figure 3: Functional organization of the brachial plexus and formation of the terminal nerves. Table 1: Distribution of the Brachial Plexus 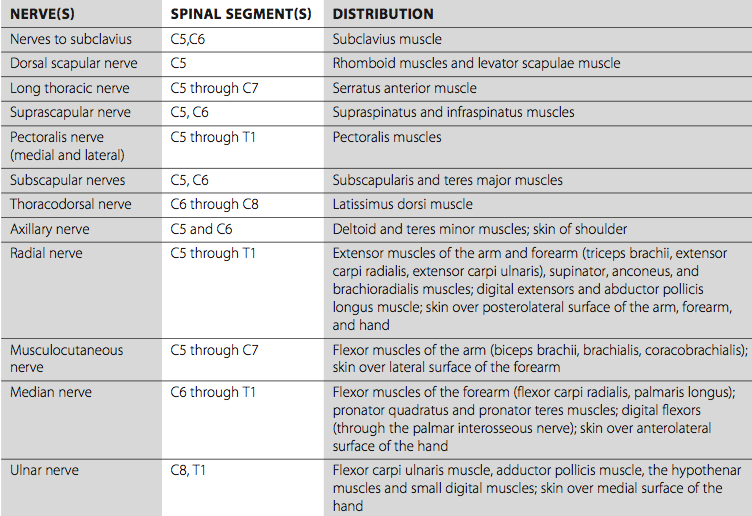 Distribution of Blockade The interscalene approach to brachial plexus blockade results in anesthesia of the shoulder, arm, and elbow (Figure 4). Note that the skin over and medial to the acromion is supplied by the supraclavicular nerve, which is a branch of the cervical plexus. Supraclavicular nerves are usually blocked with the brachial plexus when an interscalene block is performed. This is because the local anesthetic invariably spills over from the interscalene space into the prevertebral fascia and blocks the branches of the cervical plexus. The classic interscalene block, is not recommended for hand surgery due to potential sparing of the inferior trunk and the lack of blockade of the C8 and T1 roots. Single-Injection Interscalene Block Equipment A standard regional anesthesia tray is prepared with the following equipment:
Figure 4: Sensory distribution of the brachial plexus. The innervation is shown for didactic purposes; the exact extent of anesthesia with interscalane block varies considerably and often spares the hand. Landmarks and Patient Positioning The patient is in a supine or semi-sitting position with the head facing away from the side to be blocked (Figure 5). The arm should rest comfortably on the bed, abdomen, or arm-board to allow detection of responses to nerve stimulation. Removal of a cast (when present) can help to detect motor response, although removal is not essential because the responses to nerve stimulation are usually mixed (stimulation of trunks and divisions rather than specific nerves) and proximal motor response is adequate (e.g., deltoid, pectoralis). These are the primary landmarks for performing this block: 1. The clavicle 2. Posterior border of the clavicular head of the sternocleidomastoid muscle 3. External jugular vein (usually crosses the interscalene groove at the level of the trunks)
Maneuvers to Facilitate Landmark Identification Identification of the interscalene groove can be made easier by performing the following steps:
Technique After cleaning the skin with an antiseptic solution, 1 to 3 mL of local anesthetic is infiltrated subcutaneously at the determined needle insertion site. The fingers of the palpating hand should be gently but firmly pressed between the anterior and middle scalene muscles to shorten the skin-brachial plexus distance. The skin over the neck can be very mobile, and care should be taken to stabilize the fingers as well as to stretch the skin gently between the two fingers to ensure accuracy in needle advancement and redirection. The palpating hand should not be allowed to move during the entire block procedure to allow for precise redirection of the needle when necessary. The needle is inserted 3-4 cm (approximately 2 finger-breadths) above the clavicle and advanced at an angle almost perpendicular to the skin plane (Figure 7).
Figure 7: Needle insertion for interscalene brachial plexus block. The needle is inserted between fingers posi- tioned in the interscalene groove with a slight caudad ori- entation to decrease the chance of entrance in the cervical spinal cord. White arrow: insertion of the sternal head of the sternocleidomastoid muscle. Red arrows: posterior border of the sternocleidomastoid muscle. Blue arrow: external jugular vein. The insertion point for the block is often immediately posterior to the external jugular vein. The needle must never be oriented cephalad; a slight caudal orientation reduces a chance for an inadvertent insertion of the needle into the cervical spinal cord. The nerve stimulator should be initially set to deliver 0.8 to 1.0 mA (2 Hz, 0.1 ms). The needle is advanced slowly until stimulation of the brachial plexus is obtained. This typically occurs at a depth of 1 to 2 cm in most all patients. Once appropriate twitches of the brachial plexus are elicited, 25 to 35 mL of local anesthetic are injected slowly with intermittent aspiration to rule out intravascular injection. This "low-interscalene" approach differs from the classic description of the interscalene block, which uses the cricoid cartilage as a landmark. The principal advantage to the low approach is that the brachial plexus is more compact at the lower levels, and reliable coverage of the upper, middle, and lower trunks can be achieved with a single injection (Figure 8). In contrast, the classic approach may spare the lower trunk, which limits its use for forearm and elbow surgery. When insertion of the needle does not result in upper extremity muscle stimulation, the following maneuvers can be used (Figure 9): 1. Keep the palpating hand in the same position and the skin between the fingers stretched 2. Withdraw the needle to the skin level, redirect it 15° posteriorly, and repeat the needle advancement. 3. Withdraw the needle to the skin level, redirect it 15° anteriorly, and repeat the needle insertion.
Figure 8: Distribution of the mixture of local anesthetic and a radiopaque contrast after an interscalene brachial plexus injection. The arrows and the circle indicate "negative" contrast image of the roots of the brachial plexus.
Figure 9: Maneuvers to obtain a motor response of the brachial plexus during electric nerve localization. When the motor response is not obtained on the initial needle pass, the needle is redirected anteriorly or posteriorly to the original insertion plane as shown in the figure. Troubleshooting Table 2: Common Problems During Nerve Localization and the Corrective Action 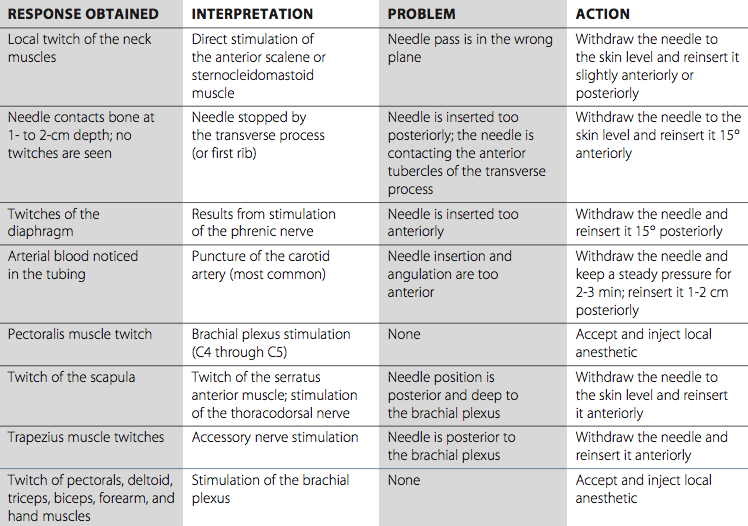
Block Dynamics and Perioperative Management When stimulation with a low-intensity current and slow needle advancement are used, interscalene brachial plexus block is associated with minor patient discomfort. Excessive sedation is not only unnecessary but also potentially disadvantageous because patient cooperation during landmark assessment and block performance is beneficial. The administration of benzodiazepines also may decrease the tone of the scalene and sternocleidomastoid muscles, making their recognition more difficult. We typically use small doses of midazolam (e.g., 1-2 mg) and/or short acting opioid (e.g., alfentanyl 250-500 mcg), so that the patient is comfortable and cooperative during nerve localization. The onset time of this block is relatively short. The first sign of the blockade is typically a loss of coordination of the shoulder and arm muscles. This sign is seen sooner than the onset of a sensory blockade or a temperature change and, when observed within 1 to 2 minutes after injection, is highly predictive of a successful brachial plexus blockade. In patients undergoing shoulder arthroscopic procedures, it is important to note that the arthroscopic portals are often inserted outside the cutaneous distribution of the interscalene block. Local infiltration at the site of the incision by the surgeon is all that is needed because the entire shoulder joint and deep tissues are anesthetized with the interscalene block alone. Education of the patient regarding block effects and side effects is important with interscalene block. Patients should be instructed to take prescribed oral analgesics and use ice packs before the block resolves. This regimen is of particular importance with ambulatory patients who may experience significant pain after discharge if they are unprepared.
Continuous Interscalene Block A continuous interscalene block is a more advanced regional anesthesia technique, and adequate experience with the single-injection technique is necessary. Paradoxically, although a single-injection interscalene block is one of the easiest intermediate techniques to perform and master, placement of the catheter can be one of the more technically challenging procedures. This is because the shallow position of the brachial plexus does not allow for an easy needle stabilization during catheter advancement and catheters can easily get dislodged during needle withdrawal. Otherwise, the technique is similar to the single-injection procedure, apart from a slight difference in the angle of the needle. This procedure provides excellent analgesia in patients following shoulder, arm, and elbow surgery. Equipment A standard regional anesthesia tray is prepared with the following equipment:
Kits come in two varieties based on catheter construction: nonstimulating (conventional) and stimulating catheters. During the placement of a conventional nonstimulating catheter, the stimulating needle is first advanced until appropriate twitches are obtained. Then, 5 to 10 mL of local anesthetic or other injectate (e.g., dextrose 5% in water) can be injected to "open up" a space for the catheter to advance freely without resistance. The catheter is then inserted through the needle approximately 3 to 5 cm beyond the tip of the needle. The needle is withdrawn, the catheter is secured, and the remaining local anesthetic is injected via the catheter. Stimulating catheters are insulated and have a filament or core that transmits current to a bare metal tip. After obtaining twitches with the needle, the catheter is advanced with the nerve stimulator connected until the anesthesiologist is satisfied with the quality of the motor response. If the twitch is lost, the catheter may be withdrawn until it reappears, and the catheter is readvanced. This method requires no conducting solution to be injected through the needle (i.e., local anesthetic, saline) before catheter advancement, or difficulty obtaining a motor response will result. Landmarks and Patient Positioning The patient is in the same position as for the single-injection technique. However, it is imperative that the anesthesiologist assume an ergonomic position to allow maneuvering during catheter insertion. It is often easiest for the clinician to stand at the head of the bed to avoid inserting the needle at an awkward angle because it is desirable to advance the catheter in an inferolateral direction (i.e., the same direction as the plexus). It is also important that all equipment, including the catheter, be immediately available and prepared in advance because small movements of the needle that might occur while trying to prepare the catheter can result in dislodging the needle from its position in the brachial plexus sheath. The landmarks for a continuous interscalene brachial plexus block are similar to those for the single-shot technique: 1. Clavicle 2. Posterior border of the clavicular head of the sternocleidomastoid muscle 3. External jugular vein Technique 
Figure 10: Insertion of a catheter into the interscalene space. Insertion of the catheter often requires lowering of the needle angle to facilitate catheter passage. Catheters are typically inserted 3-5 cm past the needle tip to prevent inadvertent removal. The subcutaneous tissue at the projected site of needle inser- tion is anesthetized with local anesthetic. The block needle is attached to a nerve stimulator (1.0 mA, 2 Hz, 0.1 ms). With this technique, the palpating hand must firmly stabilize the skin to facilitate needle insertion and insertion of the catheter. A 3- to 5-cm block needle is inserted in the interscalene groove, with a more pronounced caudal angle than the single-shot technique, and advanced until the brachial plexus twitch is elicited at 0.2 to 0.5 mA. Precautions should be taken to avoid inserting the needle through the external jugular vein because this invariably results in prolonged oozing from the site of puncture. This can be avoided by retracting the external jugular vein and inserting the needle slightly in front of or posteriorly to the external jugular vein. Paying meticulous attention to the position of the needle, the catheter is inserted no more than 3 to 5 cm beyond the tip of the needle (Figure 10). The catheter is secured using an adhesive skin preparation such as benzoin, followed by application of a clear dressing. Several securing devices are also commercially available. The infusion port should be clearly marked "continuous nerve block," and the catheter should be carefully checked for intravascular placement before administering a bolus or infusion of local anesthetics.
Management of the Continuous Infusion Continuous infusion is initiated after an initial bolus of dilute local anesthetic is administered through the needle or catheter. For this purpose, we routinely use 0.2% ropivacaine 15 to 20 mL. Diluted bupivacaine or levobupivacaine are suitable also but can result in greater motor blockade. Other adjuvants (clonidine, epinephrine, or opioids) do not appear to be of benefit in continuous nerve blocks. The infusion is maintained at 5 mL/h when a dose of patient-controlled regional analgesia (PCRA) (5 mL every 30-60 minutes) is planned. Inpatients should be seen and instructed on the use of PCRA at least once a day. During each visit, the insertion site should be checked for erythema and swelling and the extent of motor and sensory blockade documented. The infusion and PCRA dose should be adjusted accordingly. When the patient complains of breakthrough pain, the extent of the blockade should be checked first. A bolus of dilute local anesthetic (e.g., 10-15 mL of 0.2% ropivacaine) can be injected to reactivate the catheter. Increasing the infusion rate alone never results in improvement in analgesia. When the bolus fails to result in blockade after 30 minutes, the catheter should be considered to have migrated and should be removed. Alternatively, where equipment and expertise is available, the position of the catheter can be confirmed ultrasonographically by documenting the location of an injection bolus through the catheter. Every patient receiving a continuous nerve block infusion should be prescribed an immediately available alternative pain management protocol because incomplete analgesia and catheter dislodgment can occur. Complications of interscalane brachial plexus blocks and means of their prevention are listed in Table 3. Table 3: Complications and How to Avoid Them 
|
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)
![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)


























Post your comment