Continuous Thoracic Paravertebral Block
|
Overview 
General Considerations Continuous thoracic paravertebral blockade is an advanced regional anesthesia technique and adequate experience with the single-shot technique is a prerequisite. The continuous thoracic paravertebral block technique is more suitable for analgesia than for surgical anesthesia. The resultant blockade can be thought of as a unilateral continuous thoracic epidural, except that there are no significant hemodynamic changes. The technique is somewhat similar to the single-shot injection, except that the needle should be properly angled to allow for insertion of the catheter. This technique provides excellent analgesia and it is devoid of significant hemodynamic effects in patients after mastectomy and unilateral chest surgery. Regional Anesthesia Anatomy 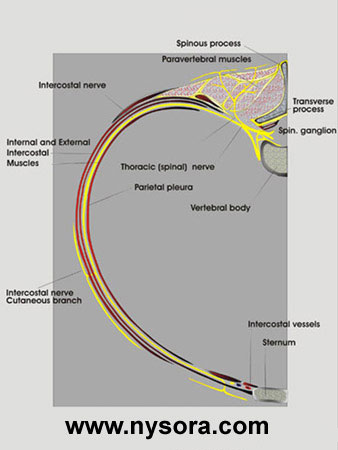 The thoracic paravertebral space is a wedge-shaped area that lies on either side of the vertebral column. Its walls are formed by the parietal pleura anterolaterally; vertebral body, the intervertebral disk, and intervertebral foramen medially; and the superior costotransverse process posteriorly. The spinal nerves in the paravertebral space are organized in small bundles submerged in the fat of the area. At this location, the spinal nerves are not enveloped by a thick fascial sheath. Therefore, they are relatively easily anesthetized by injection of local anesthetic. The thoracic paravertebral space is continuous, with the intercostal space laterally, epidural space medially, and the contralateral paravertebral space via the prevertebral fascia. The mechanism of action of a paravertebral blockade includes direct penetration of the local anesthetic into the spinal nerve, extension laterally along with the intercostal nerve, and medial extension through the intervertebral foramina. Distribution of Anesthesia  Thoracic paraverterbral blockade results in ipsilateral dermatomal anesthesia. The location of the resulting dermatomal distribution of anesthesia or analgesia is a function of the level blocked and the volume of local anesthetic injected. Patient Positioning  The patient is positioned in the supine or lateral decubitus position. Most of our patients with this block are patients undergoing various thoracic procedures. For practical reasons, most catheters are placed postoperatively, just before the patients emerge from general anesthesia. Since these patients are typically already positioned in the lateral decubitus position, this practice precludes the need for special patient positioning or premedication for the block placement. In addition, the risk of pneumothorax is nonexistent because the patients already have a chest tube inserted. However, the ability to clearly visualize spinous processes is of crucial importance. Equipment  A standard regional anesthesia tray is prepared with the following equipment: Landmarks  The landmarks for continuous paravertebral block are identical to those in the single-shot technique:
Technique  The subcutaneous tissues and paravertebral muscles are infiltrated with local anesthetic to decrease the discomfort at the site of needle insertion. The needle is attached to a syringe with local anesthetic and advanced in a saggital and slightly cephalad plane to contact the transverse process.  Once the transverse process is contacted, the needle is withdrawn back to the skin and reinserted with a 10°-15° cephalad angle to "walk off" 1 cm past the transverse process and enter the paravertebral space. As the paravertebral space is entered, a certain "give" is sometimes perceived, but it should not be relied upon as the target. Once the paravertebral space is entered, the initial bolus of local anesthetic (5-6 mL) is first injected through the needle. The catheter is inserted some 5 cm beyond the needle tip.  The catheter is then secured using a solution of benzoin and clear occlusive dressing and clearly labeled "paravertebral nerve block catheter." The catheter should be carefully checked for air, CSF, and blood before dosing a local anesthetic or starting the continuous infusion.
Management of the Continuous Infusion Continuous infusion is initiated after an initial bolus of dilute local anesthetic is administered through the catheter. The bolus injection consists of a small volume of 0.5% ropivacaine or bupivacaine (e.g., 8 mL). For continuous infusion, 0.2% ropivacaine, or 0.25% bupivacaine (l-bupivacaine) are suitable. The local anesthetic is infused at 10 mL/hr or 6 mL/hr when a PCA dose is planned (4 mL/q30 minutes).
Choice of Local Anesthetic It is almost always beneficial to achieve longer acting anesthesia/analgesia in thoracic paravertebral blockade by using longer acting local anesthetic. Unless lower lumbar levels (L2-5) are planned to be blocked, paravertebral blocks do not result in motor block of an extremity and do not impair patient's ability to ambulate or take care of themselves. In addition, relatively small volumes injected at several levels do not present a concern for local anesthetic toxicity.
Block Dynamics and Perioperative Management Placement of the paravertebral block is associated with moderate patient discomfort. Adequate sedation (midazolam 2-4mg) is always necessary to facilitate placement of the block. We also routinely administer alfentanyl 250-750 µg just before beginning the block procedure. However, excessive sedation should be avoided because the positioning becomes difficult when patients cannot keep their balance in the sitting position. The blockade depends on anesthetic dispersion within the space to reach the individual roots at the level of the injection. The first sign of the blockade is the loss of pin-prick sensation at the dermatomal distribution of the root being blocked. The higher the concentration and volume of the local anesthetic used, the faster the onset can be expected. Complications and How to Avoid Them
Bibliography 1. Buckenmaier CC 3rd, Steele SM, Nielsen KC, Martin AH, Klein SM: Bilateral continuous paravertebral catheters for reduction mammoplasty. Acta Anaesthesiol Scand 2002; 46:1042-5. 2. Catala E, Casas JI, Unzueta MC, Diaz X, Aliaga L, Villar Landeira JM: Continuous infusion is superior to bolus doses with thoracic paravertebral blocks after thoracotomies. J Cardiothorac Vasc Anesth 1996; 10:586-8. 3. Cheung SL, Booker PD, Franks R, Pozzi M: Serum concentrations of bupivacaine during prolonged continuous paravertebral infusion in young infants. Br J Anaesth 1997; 79:9-13. 4. Eng J, Sabanathan S: Continuous paravertebral block for postthoracotomy analgesia in children. J Pediatr Surg 1992; 27:556-7. 5. Johnson LR, Rocco AG, Ferrante FM: Continuous subpleural-paravertebral block in acute thoracic herpes zoster. Anesth Analg 1988; 67:1105-8. 6. Ganapathy S, Murkin JM, Boyd DW, Dobkowski W, Morgan J: Continuous percutaneous paravertebral block for minimally invasive cardiac surgery. J Cardiothorac Vasc Anesth 1999; 13:594-6. 7. Hultman JL, Schuleman S, Sharp T, Gilbert TJ: Continuous thoracic paravertebral block. J Cardiothorac Anesth 1989; 3:54. 8. Karmakar MK, Booker PD, Franks R: Bilateral continuous paravertebral block used for postoperative analgesia in an infant having bilateral thoracotomy. Paediatr Anaesth 1997; 7:469-71. 9. Richardson J, Sabanathan S, Jones J, Shah RD, Cheema S, Mearns AJ: A prospective, randomized comparison of preoperative and continuous balanced epidural or paravertebral bupivacaine on post-thoracotomy pain, pulmonary function and stress responses. Br J Anaesth 1999; 83:387-92. |
| 12/19/2015(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/24/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../../../files/bk-nysora-ad.jpg)


















Post your comment