Electrical Nerve Stimulators and Localization of Peripheral Nerves
Ali Nima Shariat, Patrick M. Horan, Kimberly Gratenstein, Colleen McCally, and Ashton P. Frulla
|
History of Electrical Nerve Stimulation Quick Facts 1780: Galvani (1) was the first to describe the effect of electrical neuromuscular stimulation The use of nerve stimulation became commonplace in clinical practice only in the mid- to late 1990s. Research on the needle-nerve relationship and the effect of stimulus duration ensued. (9-11) More recently, the principles of electrical nerve stimulation were applied to surface mapping of peripheral nerves using percutaneous electrode guidance (PEG) (12-15) for confirmation and epidural catheter placement (16-18) and peripheral catheter placement (19). This chapter discusses the electrophysiology of nerve stimulation, electrical nerve stimulators, various modes of localization of peripheral nerves, and integration of the technology into the realm of modern regional anesthesia. What is Peripheral Electrical Nerve Stimulation? Nerve stimulation is a commonly used method for localizing nerves before the injection of local anesthetic. Electrical nerve stimulation in regional anesthesia is a method of using a low-intensity (up to 5 mA) and short-duration (0.05-1 ms) electrical stimulus (at 1-2 Hz repetition rate) to obtain a defined response (muscle twitch or sensation) to locate a peripheral nerve or nerve plexus with an (insulated) needle. The goal is to inject a certain amount of local anesthetic in close proximity to the nerve to block nerve conduction and provide a sensory and motor block for surgery and/or, eventually, analgesia for pain management. The use of nerve stimulation can also help to avoid an intraneural intrafascicular injection and, consequently, nerve injury. Electrical nerve stimulation can be used for a single-injection technique, as well as for guidance during the insertion of continuous nerve block catheters. More recently, ultrasound (US) guidance and, in particular, the so-called dual guidance technique in which both techniques (peripheral nerve stimulation [PNS] and US) are combined, has become a common practice in many institutions. Indications for the Use of PNS In principle, almost all plexuses or other larger peripheral nerves can be located using PNS. (20) The goal of nerve stimulation is to place the tip of the needle (more specifically, its orifice for injection) in close proximity to the target nerve to inject the local anesthetic in the vicinity of the nerve. The motor response (twitch) to PNS is objective and reliable and independent from the patient's (subjective) response. Nerve stimulation is often helpful to confirm that the structure imaged with ultrasound (US) is actually the nerve that is sought. This is because the needle-nerve relationship may not always be visualized on US; an unexpected motor response can occur, alerting the operator that the needle tip is already in close proximity to the nerve. Likewise, the occurrence of a motor response at a current intensity of The disadvantages of PNS are the need for additional equipment (nerve stimulator and insulated needles), the greater cost of insulated needles, and abnormal physiology or anatomy where it may be difficult to elicit a motor response.
Basics of Neurophysiology and Electrophysiology Membrane Potential, Resting Potential, Depolarization, Action Potential, and impulse Propagation 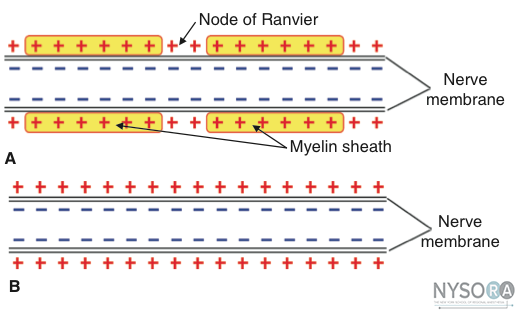 Figure 1: A) Schematic anatomic and electrophysiologic structure of nerve fibers of myelinated and (B) unmyelinated nerve fibers. All living cells have a membrane potential (a voltage potential across their membrane, measured from the outside to the inside), which varies (depending on the species and the cell type) from about -60 mV to -100 mV. Nerve and muscle cells in mammals typically have a membrane potential (resting potential) of about -90 mV. Only nerve and muscle cells have the capability of producing uniform electrical pulses, the so-called action potentials (also called spikes), which are propagated along their membranes, especially along the long extensions of nerve cells (nerve fibers, axons). A decrease in the electric potential difference (e.g., from -90 mV to -55 mV, or depolarization) elicits an action potential. If the depolarization exceeds a certain threshold, an action potential or a series of action potentials is generated by the nerve membrane (also called firing) according to the all-or-nothing rule, resulting in propagation of the action potential along the nerve fiber (axon). To depolarize the nerve membrane from outside the cell (extracellular stimulation), the negative polarity of the electrical stimulus is more effective in removing the positive charge from the outside of the membrane. This in turn decreases the potential across the membrane toward the threshold level. There are several types of nerve fibers. Each fiber type can be distinguished anatomically by their diameter and degree of myelinization. Myelinization is formed by an insulating layer of Schwann cells wrapped around the nerve fibers. These characteristics largely determine the electrophysiologic behavior of different nerve fibers, that is, the speed of impulse propagation of action potentials and the threshold of excitability. Most commonly, the distinguishing features are motor fibers (e.g., A, Aβ) and pain fibers (C). The Aα motor fibers have the largest diameter and highest degree of myelinization and therefore the highest speed of impulse propagation and a relatively low threshold level to external stimulation. C-fibers (which transmit severe, dull pain) have very little to no myelinization and are of smaller diameter. Consequently, the speed of propagation in these fibers is relatively low, and the threshold levels to external stimulation, in general, are higher. There are several other, efferent fibers, which transmit responses from various skin receptors or muscle spindles (Ad). These are thinner than Aα fibers and have less myelinization. Some of these (afferent) sensory fibers, having a relatively low threshold level, transmit the typical tingling sensation associated with a lower level of pain sensation when electrically stimulated. Such sensation can occur during transcutaneous stimulation before a motor response is elicited. The basic anatomic structure of myelinated Aα fibers (motor) and nonmyelinated C fibers (pain) is shown schematically in Figure 1. The relationship between different stimuli and the triggering of the action potential in motor and pain fibers is illustrated in Figures 2A, B. Threshold Level, Rheobase, Chronaxy A certain minimum current intensity is necessary at a given pulse duration to reach the threshold level of excitation. The lowest threshold current (at infinitely long pulse durations) is called rheobase. The pulse duration (pulse width) at double the rheobase current is called chronaxy. Electrical pulses with the duration of the chronaxy are most effective (at relatively low amplitudes) to elicit action potentials. This is the reason why motor response can be elicited at such short pulse duration (e.g., 0.1 ms) at relatively low current amplitudes while avoiding the stimulation of C-type pain fibers. Typical chronaxy figures are 50 to 100 μs (Aα fibers), 170 μs (AΔ fibers), and ≥400 μs (C fibers). Figure 3 illustrates the relationship of the rheobase to chronaxy for motor fibers versus pain nerve fibers. Impedance, Impulse Duration, and Constant Current The electrical circuit is formed by the nerve stimulator, the nerve block needle and its tip, the tissue characteristics of the patient, the skin, the skin electrode (grounding electrode), and the cables connecting all the elements. The resistance of this circuit is not just a simple Ohm's resistor equation because of the specific capacitances of the tissue, the electrocardiogram (ECG) electrode to skin interface, and the needle tip, which influence the overall resistance. The capacitance in the described circuit varies with the frequency content of the stimulation current, and it is called impedance, or a so-called complex resistance, which depends on the frequency content of the stimulus. In general, the shorter the impulse, the higher its frequency content, and, consequently, the lower the impedance of a circuit with a given capacitance. Conversely, a longer pulse duration has a lower frequency content. As an example, for a 0.1-ms stimulus, the main frequency content is 10 kHz plus its harmonics; whereas for a 1.0-ms impulse, the main frequency content is 1 kHz plus harmonics. In reality, the impedance of the needle tip and the electrode to skin impedance have the highest impact. The impedance of the needle tip largely depends on the geometry and insulation (conductive area). The electrode to skin impedance can vary considerably between individuals (e.g., type of skin, hydration status) and can be influenced by the quality of the ECG electrode used. Because of the variable impedance in the circuit, created primarily by the needle tip and electrode to skin interface, a nerve stimulator with a constant current source and sufficient (voltage) output power is important to use to compensate for the wide range of impedances encountered clinically. 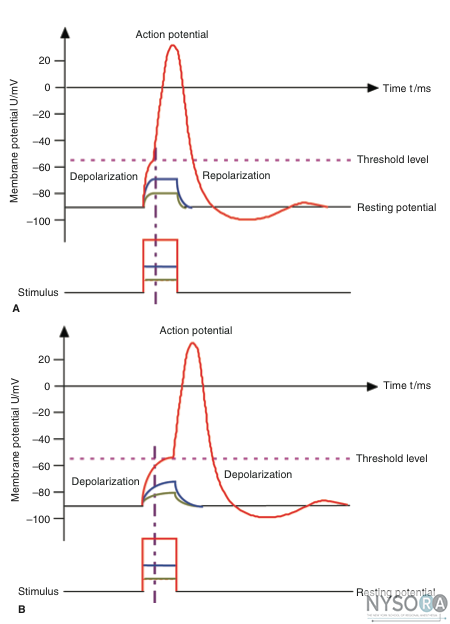
(A) Action potential, threshold level, and stimulus. Motor fibers have a short chronaxy because of the relatively low capacitance of their myelinated membrane (only the area of the nodes of Ranvier count; see Figure 1), therefore, it takes only a short time to depolarize the membrane up to the threshold level. (B) Pain fibers have a long chronaxy because of the higher capacitance of their nonmyelinated membrane (the entire area of the membrane counts); therefore, it takes a longer time to depolarize the membrane up to the threshold level. Short impulses (as indicated by the vertical dotted line) would not be able to depolarize the membrane to its threshold level. Clinical Use of PNS Proper Setup and Check of the Equipment The following are a few important aspects for successful electrolocalization of the peripheral nerves using PNS: - Use a high-quality nerve stimulator and a high accuracy constant current source - Use insulated nerve stimulation needles with a small conductive area at the tip. The smaller the conductive area, the higher the current density is at the tip, and the greater spatial discrimination in the near field. - Use high-quality skin electrodes with a low impedance - Before starting the procedure, check for the proper functioning of the nerve stimulator and the connecting cables. - During nerve stimulator-assisted nerve localization, the negative pole (cathode) should be connected to the stimulating electrode (needle) and the positive pole (anode) to the patient's skin. - The design of the connectors should prevent a faulty polarity connection. - Connect the nerve stimulation needle to the nerve stimulator (which should be turned on), and set the current amplitude and duration to the desired levels. - For superficial blocks, select 1.0 mA as a starting current intensity. - For deep blocks, select 1.5 mA as a starting current intensity. - Select between 0.1 and 0.3 ms of current duration for most purposes. - For more technical details and how to operate a specific nerve stimulator, refer to the instructions for use supplied with the stimulator.
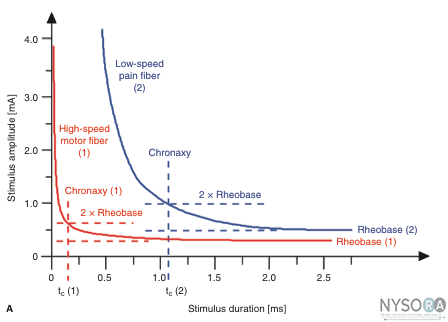 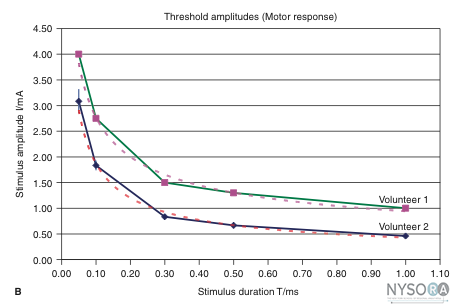 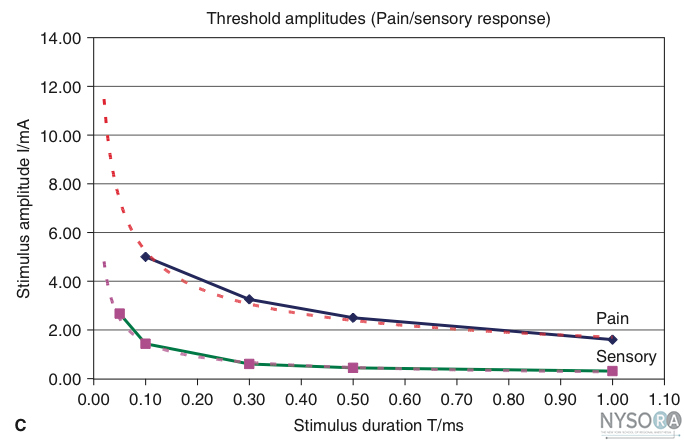
Figure 3: (A) Comparison of threshold curves, chronaxy, and rheobase level of motor (high speed) and pain fibers (low speed). (B) Experimental data, threshold amplitudes obtained with percutaneous stimulation (Stimuplex Pen and Stimuplex HNS 12). Stimulation obtained with percutaneous stimulation of the median nerve near the wrist looking for motor response of the thumb. (C) Experimental data, threshold amplitudes obtained with percutaneous stimulation (Stimuplex Pen and Stimuplex HNS 12). Stimulation of the median and radial nerves near the wrist and at the midforearm looking for electric paresthesia (tingling sensation) in the middle and ring finger (median nerve) or superficial pain sensation near the wrist (radial nerve), respectively. Transcutaneous Nerve Mapping  Figure 4: Tip configuration of several commercially available nerve mapping peripheral nerve stimulators. From left to right: Stimuplex Pen, B. Braun Melsungen (Germany); nerve mapping pen, Pajunk (Germany); NeuroMap, HDC (USA).c toxicity Electrolocalization of peripheral nerves is typically accomplished by inserting a needle into the tissue and advancing the needle toward the expected location of the nerve(s) of interest. However, a nerve mapping pen can be used to locate superficial nerves (up to a maximum depth of approximately 3 cm) with transcutaneous nerve stimulation before the nerve block needle is inserted. Transcutaneous nerve mapping is particularly useful when identifying the best site for needle insertion in patients with difficult anatomy or when the landmarks prove difficult to indentify. Figure 4 shows three examples of commercially available nerve mapping pens. Nerve mapping is also very useful when training anesthesia residents. It should be noted that longer stimulus duration (e.g., 1 ms) is needed to accomplish transcutaneous nerve stimulation, because the energy required to stimulate transcutaneously is larger. The electrode tip of the pen should have an atraumatic ball-shaped tip. The conductive tip diameter should not be larger than approximately 3 mm to provide sufficient current density and spatial discrimination, which may not be the case with larger tip diameters. Some nerve stimulators do not provide the required impulse duration of 1 ms or a strong enough constant current source (5 mA at minimum 12-kOhm output load) to perform nerve mapping. Therefore, it is recommended that the mapping pen and the nerve stimulator be paired, ideally by acquiring them from the same manufacturer. The transcutaneous stimulation often results in a sensation reported by the patient as tingling, pinprick, or a slight burning sensation. The perception varies greatly among individuals. Most people tolerate transcutaneous stimulation with a nerve mapping pen very well; however, some individuals describe it as uncomfortable or even painful (depending on the stimulus amplitude and duration). However, the amount of energy delivered by nerve stimulators with a maximum output of 5 mA at 1 msec pulse duration is far too low to create any injury of the skin or the nerves. A moderate premedication is usually sufficient to make the procedure well tolerated by patients. Percutaneous Electrode Guidance  Figure 5: Percutaneous electrode guidance technique using Stimuplex Guide (B. Braun Melsungen, Germany) during a vertical infraclavicular block procedure. PEG (10,11) combines the transcutaneous nerve stimulation (nerve mapping) with nerve block needle guidance (Figure 5). In essence, a small aiming device is mounted and locked onto a conventional nerve block needle, which allows the conductive needle tip to make contact with the skin without scratching or penetrating the skin. Once the best response is obtained, the needle is advanced through the skin in the usual fashion and the remainder of the apparatus continues to stabilize the needle and guide it toward the target. The device also allows the operator to make indentations in the skin and tissue so the initial distance between the needle tip at the skin level and the target nerve is reduced and the nerve block needle has less distance to travel through tissue. The technique allows for prelocation of the target nerve(s) before skin puncture. Operating the Nerve Stimulator The starting amplitude used for nerve stimulation depends on the local practice and the projected skin-nerve depth. For superficial nerves, amplitude of 1 mA at 0.1 (or 0.3) ms impulse duration to start is chosen in most cases. For deeper nerves, it may be necessary to increase the initial current amplitude between 1.5 and 3 mA until a muscle response is elicited at a safe distance from the nerve. Too high current intensity, however, can lead to direct muscle stimulation or discomfort for the patient, both of which are undesirable. Once the sought-after muscle response is obtained, the current intensity amplitude is gradually reduced and the needle is advanced further slowly. The needle must be advanced slowly to avoid too rapid advancement between the stimuli. Advancement of the needle and current reduction are continued until the desired motor response is achieved with a current of 0.2-0.5 mA at 0.1 ms stimulus duration. The threshold level and duration of the stimulus are interdependent; in general, a short pulse duration is a better discriminator of the distance between the needle and the nerve. (20) When the motor twitch is lost during needle advancement, the stimulus intensity first should be increased to regain the muscle twitch rather than move the needle blindly. Once a proper motor response is obtained with a current of 0.2-0.5 mA (most nerve blocks), the needle is positioned correctly for an injection of local anesthetic. A small test dose of local anesthetic is injected, which abolishes the muscle twitch. Then the total amount of local anesthetic appropriate for the desired nerve block is injected. Of note, the highly conductive injectate (e.g., local anesthetic or normal saline solution) short-circuits the current to the surrounding tissue, effectively abolishing the motor response. In such situations, increasing the amplitude may not bring back the muscle twitch. Tsui and Kropelin (21) demonstrated that injection of dextrose 5% in water (D5W) (which has a low conductivity) does not lead to loss of the muscle twitch if the needle position is not changed. It should be remembered that the absence of the motor response with a stimulating current even up to 1.5 mA does not rule out an intraneural needle placement (low sensitivity). However, the presence of a motor response with a low-intensity current ( To avoid or minimize discomfort for the patient during the nerve location procedure, it is recommended that a too high stimulating current be avoided. The needle should not be advanced too fast because it can increase the risk of injuries and the evoked motor response may be missed.
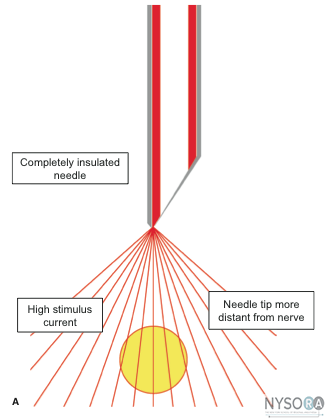
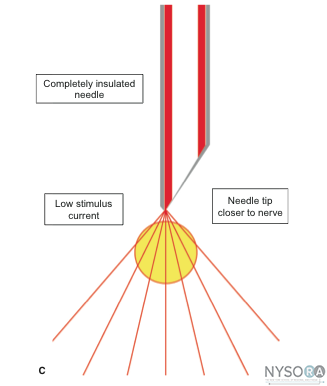 Figure 6: (A) Stimulating needle at a distance to the nerve and high stimulus current elicits a weak evoked motor response. (B) Stimulation needle close to the nerve and high stimulus current eliciting a strong muscle twitch. (C) Stimulating needle close to the nerve and low (near threshold) stimulus current elicits a strong evoked motor response. The Role of impedance Measurement Measurement of the impedance can provide additional information if the electrical circuit is optimal. Theoretically, impedance can identify an intraneural or intravascular placement of the needle tip. Tsui and colleagues (22) reported that the electrical impedance nearly doubles (12.1-23.2 kOhm), which is significant, when the needle is advanced from an extraneural to intraneural position in a porcine sciatic nerve. Likewise, injection of a small amount of (D5W), which has a high impedance, results in a significantly higher increase of impedance in the perineural tissue than it does within the intravascular space. (23) Thus measurement of the impedance before and after dextrose injection can potentially detect intravascular placement of the needle tip, thus identifying the placement before the injection of local anesthetic. In this report, the perineural baseline impedance [25.3 (± 2.0) kOhm] was significantly higher than the intravascular [17.2 (± 1.8) kOhm]. Upon injection of 3 mL of D5W, the perineural impedance increased by 22.1 (± 6.7) kOhm to reach a peak of 50.2 (± 7.6) kOhm and remained almost constant at about 42 kOhm during the 30-second injection time. By contrast, intravascular impedance increased only by 2.5 (± 0.9) kOhm, which is significantly less compared with the perineural needle position. At the present time, however, more data are needed before these findings can be incorporated as an additional safely monitoring method in clinical practice. Sequential Electrical Nerve Stimulation Current nerve stimulation uses stimuli of identical duration (typically 0.1 ms), usually at 1 or 2 Hz repetition frequency. A common problem during nerve stimulation is that the evoked motor response is often lost while moving the needle to optimize its position. In such cases, it its recommended that the operator either increase the stimulus amplitude (mA) or increase the impulse duration (ms), the latter of which may not be possible. Alternatively, the operator can take a couple of steps, depending on type of the nerve stimulator used. The SENSe (sequential electrical nerve stimulation) technique incorporates an additional stimulus with a longer pulse duration after two regular impulses at 0.1 msec duration, creating a 3 Hz stimulation frequency. (24) The third longer impulse delivers more charge than the first two and therefore has a longer reach into the tissue. Consequently, an evoked motor response often is elicited at 1 Hz, even when the needle is distant from the nerve. Once the needle tip is positioned closer to the nerve, muscle twitches are seen at 3 Hz. The advantage of the SENSe is that a motor response (at 1/second) is maintained even when the motor response previously elicited by the first target threshold amplitude remains the same as usual (about 0.3 mA) but at 3 stimuli per second. With the SENSe technique, a motor response at only 1/second indicates that the needle is not yet placed correctly. 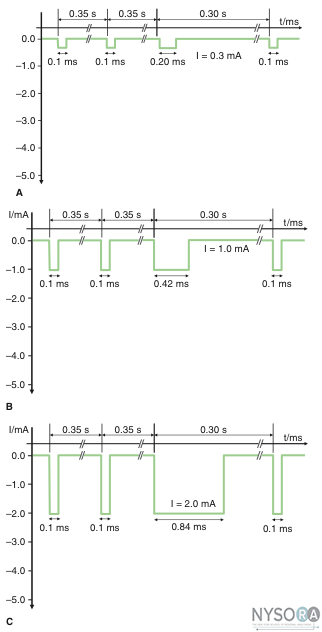
Figure 7: Sequential electrical nerve stimulation (SENSe) impulse pattern of the Stimuplex HNS 12 nerve stimulator (B. Braun Melsungen, Germany) depending on the actual stimulus amplitude. The impulse duration of the third impulse decreases with the stimulus amplitude below 2.5 mA from 1.0 ms to a minimum of 0.2 ms compared with the constant impulse duration of 0.1 ms of the first two impulses. (A) Impulse pattern at 0.3 mA (threshold level). (B) Impulse pattern at 1.0 mA. (C) Impulse pattern at 2.0 mA. Table 1: Common Problems during Electrolocalization of Nerves and Corrective Actions
Troubleshooting During Nerve Stimulation Table 1 lists the most common problems encountered during electrolocalization of the peripheral nerves and the Characteristics of the Modern Equipment for Nerve Stimulator Guided Peripheral Nerve Blocks Most Important Features of Nerve Stimulators Electrical Features - An adjustable constant current source with an operating range of 10 kOhm, minimally, output load (impedance) and ideally at ≥15 kOhm. Safety Features
Alarms/Warnings
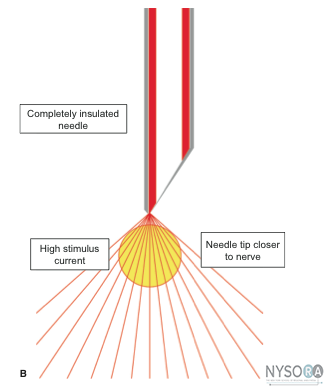
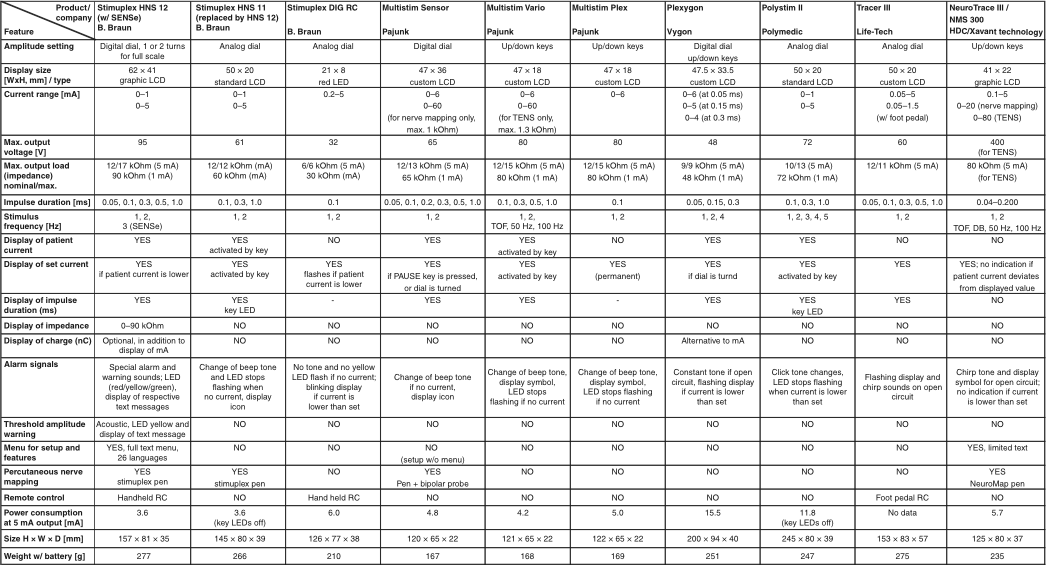
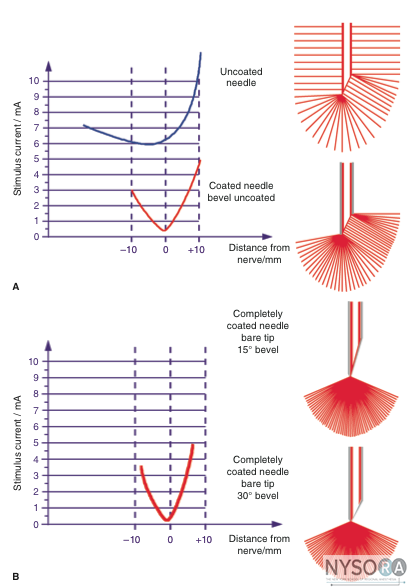
Table 2 provides a comparison of the most important features of commonly used nerve stimulators. Stimulating Needles Needle A modern stimulating needle should have the following characteristics: Figures 8A and B show a comparison of the electrical characteristics of noninsulated and insulated needles with uncoated bevel (Figure 8A) and fully coated needles with a pinpoint electrode (Figure 8B). Even though a noninsulated needle provides for discrimination (change in threshold amplitude) while approaching the nerve, there is virtually no ability to discriminate once the needle tip has passed the nerve. The discrimination near the nerve is more precise in needles with a pinpoint electrode tip (Figure 8B) compared with needles with an uncoated bevel (Figure 8A). Connectors Connectors and cables should be fully insulated and include a safety connector to prevent current leakage as well as the risk of electric charge if the needle is not connected to the stimulator. Extension tubing with a Luer lock connector should be present for immobile needle techniques. Visualization of the Needle Under Ultrasound Imaging Because US imaging is more in use (in particular with the use of the "dual guidance" technique), the importance of good visualization of the nerve block needle is becoming an additional important feature. The visibility (distinct reflection signal) of the needle tip certainly is the most important aspect because this is the part of the needle that is placed in the target area next to the nerve. However, in particular when using the in-plane approach, the visibility of the needle shaft is of interest as well because it helps to align the needle properly with the US beam and to visualize its entire length up to the target nerve. Stimulating Catheters In principle, stimulating catheters function like insulated needles. The catheter body is made from insulating plastic material and usually contains a metallic wire inside, which conducts the current to its exposed tip electrode. Such stimulating catheters are usually placed using a continuous nerve block needle, which is placed by first using nerve stimulation as described and acts as an introducer needle for the catheter. Once this needle is placed close to the nerve or plexus to be blocked, the stimulating catheter is introduced through it and the nerve stimulator is connected to the catheter. Stimulation through the catheter should reconfirm that the catheter tip is positioned in close proximity to the target nerve(s). However, it must be noted that the threshold currents with stimulating catheters may be considerably higher. Injection of local anesthetic or saline (which is frequently used to widen the space for threading the catheter more easily) should be avoided because this may increase the threshold current considerably and can even prevent a motor response. D5W can be used to avoid losing a motor response. (21) Since the ultimate test for the properly positioned catheter is the distribution of the local anesthetic, rather than evoked motor response, the role of the catheter stimulating with US-guided blocks is not clear. Table 2: Comparison of Most Relevant Features of Modern Nerve Stimulators
Recommendations for Best Practice - Adequate knowledge of anatomy Standard nerve stimulator settings for peripheral nerve blocks: - Stimulus duration: 0.1 ms for mixed nerves Nerve stimulator check: - Check battery status Needles: - Use fully insulated nerve block needles, Figure 8. End point of nerve stimulation: - Threshold current 0.2 to 0.3 mA (at 0.1 ms) To avoid discomfort for the patient and take precautions for safety: - Use a low-intensity current nerve stimulation
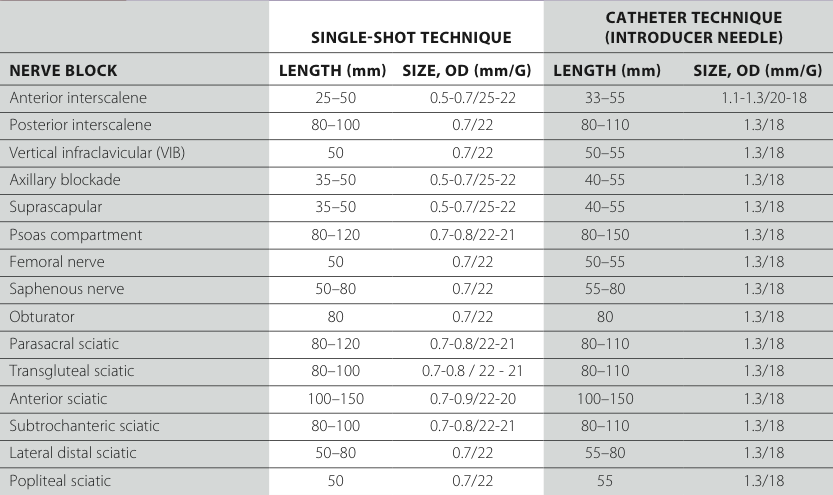
Figure 8: (A) Threshold amplitude achieved with an uncoated needle and a coated needle with an uncoated bevel. (B) Threshold amplitude achieved with a fully coated needle and a pinpoint electrode. Table 3: Stimulation Needle Sizes Recommended for Various Nerve Blocks
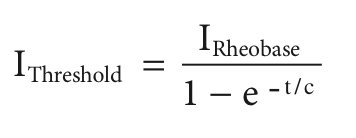
Appendix: Glossary of Physical Parameters Voltage, Potential, Current, Resistance/Impedance Voltage (U)is the difference in electrical potential between two points carrying different amounts of positive and negative charge. It is measured in volts (V) or millivolts (mV). Voltage can be compared with the filled level of a water tank, which determines the pressure at the bottom outlet (Figure 9A). In modern nerve stimulators using constant current sources, voltage is adapted automatically and cannot nor needs to be influenced by the user. Current (I)is the measure of the flow of a positive or negative charge. It is expressed in amperes (A) or milliamperes (mA). Current can be compared with the flow of water. A total charge (Q) applied to a nerve equals the product of the intensity (I) of the applied current and the duration (t) of the square pulse of the current: Q = I × t. The minimum current intensity (I) required to produce an action potential can be expressed by the relationship where, t = pulse duration, c = time constant of nerve membrane related to chronaxy.
The electrical resistance R limits the flow of current at a given voltage (see Ohm's law) and is measured in ohms (ω) or kilo Ohms (kω). If there is capacitance in addition to Ohm's resistance involved (which is the case for any tissue), the resistance becomes a so-called complex resistance, or impedance. The main difference between the two is that the value of the impedance depends on the frequency of the applied voltage/current, which is not the case for an Ohm's resistor. In clinical practice, this means the impedance of the tissue is higher for low frequencies (i.e., a long pulse duration) and lower for higher frequencies (i.e., a short impulse duration). Consequently, a constant current source (which delivers longer duration impulses, e.g., 1 ms versus 0.1 ms) needs to have a stronger output stage (higher output voltage) to compensate for the higher tissue impedance involved and to deliver the desired current. However, the basic principles of Ohm's law remain the same. Ohm's Law Ohm's lawdescribes the relationship between voltage, resis- tance, and current according to the equation:
or conversely
This means that at a given voltage, current changes with resistance. If a constant current must be achieved (as needed for nerve stimulation), the voltage has to adapt to the varying resistance of the entire electrical circuit. For nerve localization in particular, the voltage must adapt to the resistance of the needle tip, the electrode to skin interface, and the tissue layers. A constant current source does this automatically. Ohm’s law and the functional principle of a constant current source are illustrated in Figures 9A-C. Coulomb's law, Electric Field, Current Density, and Change According to Coulomb's law, the strength of the electric field and, therefore, the corresponding current density(J) in relation to the distance from the current source is given by:
This means the current (or charge) that reaches the nerve decreases by a factor of 4 if the distance to the nerve is doubled, or conversely, it increases by a factor of 4 if the distance is divided in half (ideal conditions assumed). The charge Q is the product of current multiplied by time and is given in ampere seconds (As) or coulomb (C). As an example, rechargeable batteries often have an indication of Ah or mAh as the measure of their capacitance of charge (kilo = 1000 or 103; milli = 0.001 or 10-3; micro = 0.000001 or 10-6; nano = 0.000000001 or 10-9). 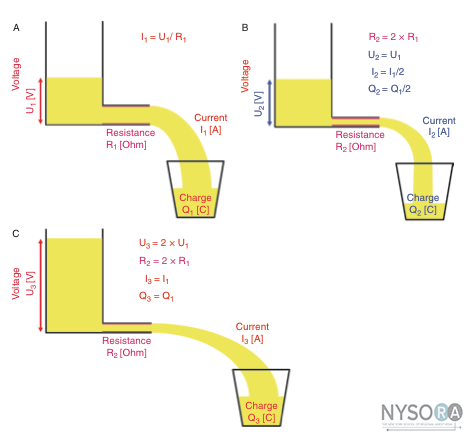
Figure 9: (A) Threshold amplitude achieved with an uncoated needle and a coated needle with an uncoated bevel. (B) Threshold amplitude achieved with a fully coated needle and a pinpoint electrode. Energy of Electrical Impulses Delivered by Nerve Stimulators and Related Temperature Effects According to a worst-case scenario calculation, the temperature increase caused by a stimulus of 5 mA current and 1 ms duration, at a maximum output voltage of 95 V, would be The maximum energy (E) of the electrical impulse deliv- ered by a common nerve stimulator would be:
The caloric equivalent for water is cw = 4.19 J g-1 K-1 One stimulus creates a temperature difference ΔT within 1 mm3 of tissue around the tip of a nerve stimulation needle. For the calculation that follows, it is assumed that tissue contains a minimum of 50% water and the mass (M) of 1 mm3 of tissue is 1 mg.
That is, the maximum temperature increase in this worstcase scenario calculation is |
![[advertisement] gehealthcare](../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../files/bk-nysora-ad.jpg)





 Educational Material Download
Educational Material Download




















Post your comment