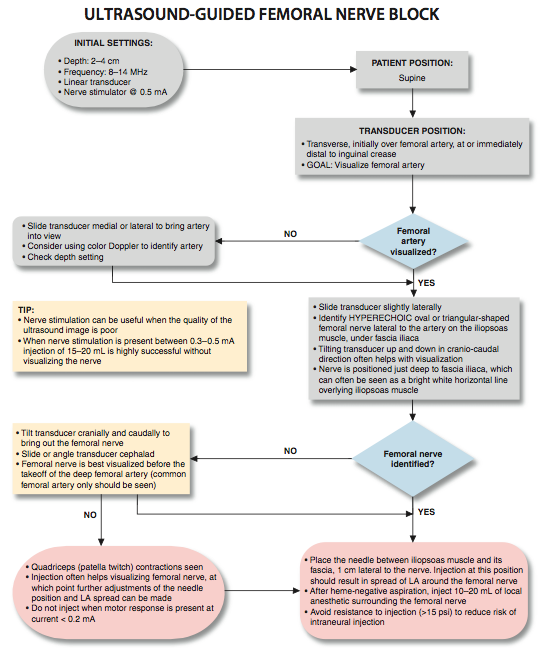
Ultrasound-Guided Femoral Nerve Block
|
Figure 1: Transducer position and needle insertion using an in-plane technique to block the femoral nerve at the femoral crease. Essentials
General Considerations The ultrasound-guided technique of femoral nerve blockade differs from nerve stimulator or landmark-based techniques in several important aspects. Ultrasound application allows the practitioner to monitor the spread of local anesthetic and needle placement and make appropriate adjustments, should the initial spread be deemed inadequate. Also, because of the proximity to the relatively large femoral artery, ultrasound may reduce the risk of arterial puncture that often occurs with this block with the use of non-ultrasound techniques. Palpating the femoral pulse as a landmark for the block is not required with ultrasound guidance, a process that can be challenging in obese patients. Although the ability to visualize the needle and the relevant anatomy with ultrasound guidance renders nerve stimulation optional, motor response obtained during nerve stimulation often provides contributory information.
Figure 2: (A) Cross-sectional anatomy of the femoral nerve (FN) at the level of the femoral crease. FN is seen on the surface of the iliopsoas muscle covered by fascia iliaca. (white arrows). Femoral artery (FA) and femoral vein (FV) are seen enveloped in their own vascular fascial sheath created by one of the layers of fascia lata. (B) Sonoanatomy of the FN at the femoral triangle. Ultrasound Anatomy  Figure 3: Obesity is a common problem in patients who present with an indication for femoral nerve block. Taping the adipose tissue away helps optimize the exposure to the femoral crease in patients with morbid obesity. Orientation begins with the identification of the pulsating femoral artery at the level of the inguinal crease. If it is not immediately recognized, sliding the transducer medially and laterally will bring the vessel into view eventually. Immediately lateral to the vessel, and deep to the fascia iliaca is the femoral nerve, which is typically hyperechoic and roughly triangular or oval in shape (Figure 2A and B). The nerve is positioned in a sulcus in the iliopsoas muscle underneath the fascia iliaca. Other structures that can be visualized are the femoral vein (medial to the artery) and occasionally the fascia lata (superficial in the subcutaneous layer). The femoral nerve typically is visualized at a depth of 2- to 4-cm. Distribution of Blockade Femoral nerve block results in anesthesia of the anterior and medial thigh down to the knee (the knee included), as well as a variable strip of skin on the medial leg and foot. It also contributes branches to the articular fibers to both the hip and knee.
 Figure 4: To image the femoral nerve and/or femoral vessels, the transducer is positioned transversely on the femoral crease as shown on the image. Equipment Equipment needed includes the following:
Landmarks and Patient Positioning This block typically is performed with the patient in the supine position, with the bed or table flattened to maximize operator access to the inguinal area. Although palpation of the femoral pulse is a useful landmark, it is not required because the artery should be readily visualized by placing the transducer transversely on the inguinal crease followed by slow movement laterally or medially. If nerve stimulation is used simultaneously, exposure of the thigh and patella are required to monitor the appropriate motor responses (patella twitch).
 Figure 5: Transducer position and needle insertion using an in-plane technique to block the femoral nerve at the femoral crease. Technique With the patient in the supine position, the skin over the femoral crease is disinfected and the transducer is positioned to identify the femoral artery and/or nerve (Figure 4). If the nerve is not immediately apparent lateral to the artery, tilting the transducer proximally or distally often helps to image and highlight the nerve from the rest of the iliopsoas muscle and the more superficial adipose tissue. In doing so, an effort should be made to identify the iliopsoas muscle and its fascia as well as the fascia lata because injection underneath a wrong fascial sheath may not result in spread of the local anesthetic in the desired plane. Once the femoral nerve is identified, a skin wheal of local anesthetic is made on the lateral aspect of the thigh 1 cm away from the lateral edge of the transducer. The needle is inserted in-plane in a lateral-to-medial orientation and advanced toward the femoral nerve (Figure 5). If nerve stimulation is used (0.5 mA, 0.1 msec), the passage of the needle through the fascia iliaca and contact of the needle tip with the femoral nerve usually is associated with a motor response of the quadriceps muscle group. In addition, a needle passage through the fascia iliaca is often felt as a "pop" sensation. Once the needle tip is witnessed adjacent (either above, below, or lateral) to the nerve (Figure 6), and after careful aspiration, 1 to 2 mL of local anesthetic is injected to confirm the proper needle placement (Figure 7). When injection of the local anesthetic does not appear to result in a spread close to the femoral nerve, additional needle repositions and injections may be necessary. In an adult patient, 10 to 20 mL of local anesthetic is adequate for a successful block (Figure 8A and B).
Continuous Ultrasound-Guided Femoral Nerve Block The goal of the continuous femoral nerve block is similar to that of the non-ultrasound-based techniques: placement of the catheter in the vicinity of the femoral nerve just deep to the fascia iliaca. The procedure consists of three phases: needle placement, catheter advancement, and securing the catheter. For the first two phases of the procedure, ultrasound can be used to ensure accuracy in most patients. The needle typically is inserted in-plane from the lateral-to-medial direction and underneath the nerve. Some clinicians prefer inserting the catheter in the longitudinal plane (inferior-to-superior), analogous to the nerve stimulation-guided technique. No data exist on whether or not one technique is superior to the other. However, the in-line approach from the lateral-to-medial has worked very well in our practice, and it is our preference because it is simpler when using ultrasound guidance.
Figure 8: (A) An actual needle path to block the femoral nerve (FN). (B) Spread of the local anesthetic (LA) within two layers of the fascia iliaca to encircle the femoral nerve (FN). FA, femoral artery.  Figure 9: Continuous femoral nerve block. Needle is seen inserted in-plane approaching the nerve from lateral to medial, although it would seem intuitive that a longitu- dinal insertion of the needle would have advantages with regard to the catheter placement. The technique demonstrated here is simpler and routinely used in our practice with consistent success. The catheter should be inserted 2-4 cm past the needle tip. The needle is advanced until the tip is adjacent to the nerve. Proper placement of the needle can be confirmed by obtaining a motor response of the quadriceps/patella, at which point 5 mL of local anesthetic is injected. This small dose of local anesthetic serves to ensure adequate distribution of the local anesthetic, as well as to make the advancement of the catheter easier. This first phase of the procedure does not significantly differ from the single-injection technique. The second phase of the procedure involves maintaining the needle in the proper position and inserting the catheter 2 to 4 cm into the space surrounding the femoral nerve (Figure 9). Insertion of the catheter can be accomplished by either a single operator or with a helper. Catheter position is observed on ultrasound as the catheter is being inserted and/or with an injection through the catheter to document its proper location. The catheter is secured by either taping it to the skin or tunneling. Preference of one technique over the other varies among clinicians, although no data exist on which one is a more secure method. The decision regarding which method to use could be based on the patient's age (no tunneling for younger patients: less mobile skin, avoidance of posttunneling scar formation), duration of the catheter therapy, and anatomy. In general, the inguinal area is quite mobile and the femoral nerve is not particularly deep, two factors that predispose to catheter dislodgment. The more lateral the starting point for needle insertion for the continuous femoral nerve block, the longer the catheter will be within the iliacus muscle, which may help prevent dislodgment because muscle tends to stabilize a catheter better than adipose tissue. Our empirical infusion regimen for femoral nerve block in an adult patient is ropivacaine 0.2% at a 5 mL/hour infusion rate and a 5 mL/hour patient-controlled bolus.
  |
| 02/20/2016(+ 2016 Dates) | |
| 01/27/2016 | |
| 03/17/2016 | |
| 04/20/2016 | |
| 09/23/2016 | |
| 10/01/2024 |
![[advertisement] gehealthcare](../files/banners/banner1_250x600/GEtouch(250X600).gif)

![[advertisement] concertmedical](../files/bk-nysora-ad.jpg)
 A
A B
B


















Post your comment