Hypertensive Crisis After A Successful Placement Of An Epidural Anesthetic In A Hypertensive Parturient
A case of a hypertensive parturient who developed a hypertensive crisis after introduction of an epidural block with 2% lidocaine solution containing epinephrine is presented.
Authors: Admir Hadzic, M.D., Jerry Vloka, M.D., Nirmal Patel, M.D and David Birnbach, M.D.
|
Abstract Background & Objectives: The use of epinephrine-containing local anesthetic solutions in pre-eclampsia is controversial. While epinephrine in local anesthetic solutions has been used without complications in this setting, a hypertensive reaction remains a concern among many clinicians. Methods: An epidural anesthetic containing epinephrine was administered to a hypertensive parturient for cesarean delivery. When a hypertensive crisis developed, the radial artery was cannulated and administration of sodium nitroprusside was initiated. Arterial blood samples were evaluated for plasma norepinephrine and serum lidocaine concentrations. Results: The introduction of lumbar epidural anesthesia for cesarean delivery using 30 mL 2% lidocaine with 1:200,000 epinephrine resulted in a profound hypertensive reaction, in a patient with pre-eclampsia, despite an adequate level of epidural anesthesia. Conclusions: Epinephrine-containing local anesthetic solutions may place a hypertensive parturient at significant risk of an acute hypertensive reaction. Reg Anesth 1995:20: 156-158. Key words: pre-eclampsia, local anesthetic solutions, lidocaine Introduction The use of epinephrine-containing local anesthetics in patients with pre-eclampsia and arterial hypertension is a continuing controversy. While epinephrine has been used without any complications in this setting, a potential for excessive hypertension after epinephrine administration is commonly cited (2,3). We present a case of hypertensive crisis in a parturient who received an epidural anesthetic using 2% lidocaine with 1:200,000 epinephrine. Norepinephrine in pcg/mL (normal = 0.0-30.0); Lidocaine in mg/L 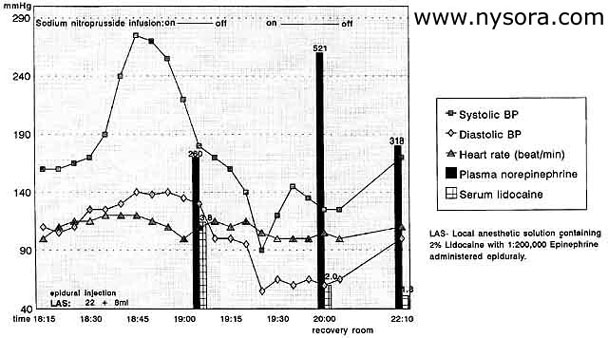 Figure 1. Blood pressure, heart rate, plasma norepinephrine, and serum lidocaine trends. Case report A 38-year-old woman, G5P2, at 36 weeks of gestation, with chronic hypertension and marginal placenta previa, presented for elective cesarean delivery. Her past medical history was significant for chronic hypertension that was controlled with verapamil 240 mg once a day. This was replaced by methyldopa 500 mg four times a day in her current pregnancy with good blood pressure control until 2 weeks prior to this admission, when she was hospitalized for 2 days with blood pressure elevated to 180/100 mm Hg. On admission, her blood pressure was noted to be 170/110 mmHg; she responded to additional doses of methyldopa and labetalol. She was 160 cm tall and weighed 80 kg, with mild pretibial edema and no hyperreflexia. The cardiovascular and respiratory system examinations were unremarkable. Her laboratory values, including coagulation profile and thyroid function tests, were within normal limits. When she entered the operating room, following an infusion of 1,500 mL of lactated Ringer's solution, her blood pressure was 160/110 mmHg with heart rate of 110 beats/min. A multiorifice epidural catheter was placed uneventfully at the L3-interspace with the patient in the sitting position, using a midline approach. On administration of 3 mL of a test dose, consisting of 1.5% lidocaine with freshly added epinephrine (1:200,000), there was no increase in heart rate on pulse oximeter or signs of a subarachnoid block. A total of 30 mL of a solution of 2% lidocaine with 1:200,000 epinephrine was incrementally given through the epidural catheter. Ten minutes after the injection of the first 22 mL of anesthetic solution, the blood pressure was 190/125 mmHg and heart rate was 115/minute. At this time the sensory level was judged to be at T-10 and an additional 8 mL was given in order to increase the level of sensory anesthesia and achieve a greater sympathetic block. Five minutes later the blood pressure rose to 275/140 mmHg and heart rate to 120/min. Labetalol 100 mg was incrementally administered intravenously with only a modest blood pressure reduction to 240/120 mmHg. The left radial artery was cannulated and a sodium nitroprusside (SNP) intravenous infusion was started, which resulted in acute blood pressure reduction to 90/50 mm Hg. This required temporary discontinuation of SNP infusion and administration of 10 mg ephedrine. At that time the patient had a definitive motor and T-4 sensory block. The right internal jugular vein was cannulated and the measured central venous pressure was 6 mm Hg. Surgery began and proceeded uneventfully, with blood pressures ranges of 130-150 mm Hg systolic and 65-80 mm Hg diastolic and heart rate of 100- 120 beats/min on a continuous infusion of SNP. The patient remained comfortable and denied intraoperative pain, without any intravenous supplementation of anesthesia. A vigorous female infant, Apgar scores of 9 at both 1 and 5 minutes, was delivered. The patient's blood pressure in the recovery room was 170/110 mmHg with a T8 sensory level. The blood pressure normalized over the next 48 hours on 240 mg verapamil daily and 200 mg labetalol twice a day, and the patient was discharged 5 days after surgery. Plasma catecholamines and serum lidocaine were sampled from the arterial line at 1-hour intervals during the surgery and on transfer to the recovery room (Figure 1). Discussion Most authors believe that pre-eclamptic patients may be more sensitive to epinephrine administration than normal parturients which can result in a worsening of hypertension.(2-5) They argue that the uterine vasculature has excessive vasoconstrictive reactivity to catecholamines,(4) and an accidental intravenous epinephrine injection can possibly have deleterious effects to both the fetus and the mother. To date, however, these complications remain only theoretical. In a series by Heller et al., epinephrine was used with lidocaine in four pre-eclamptic patients without any deterioration, and the study by Dror et al. suggested that mildly pre-eclamptic patients were not likely to experience hypertension when epinephrine is injected epidurally.(6) In our patient, the induction of epidural anesthesia with lidocaine and epinephrine resulted in an unexpected and abrupt rise of blood pressure. Most likely she had pre-eclampsia or worsening chronic hypertension, although she did not meet the strict clinical and laboratory criteria for pre-eclampsia (no generalized edema, hyperreflexia, proteinuria, uricosuria). Her normal serum creatinine, thyroid function tests, urinalysis, creatinine clearance, and urine metanephrines, argued against the most com mon forms of secondary hypertension. A routine urine screen for drugs, including cocaine, was neg ative.(7) Because pre-eclamptic patients characteristically have labile blood pressures reflecting the intense sensitivity of the vasculature to endogenous and exogenous pressers in pre-eclampsia,(8) it is possible that accidental partial intravascular injection of epinephrine resulted in an excessive catecholamine release, peripheral vasoconstriction, (4) and hypertensive crisis in this patient. However, the serial lidocaine levels, the pattern of hypertension (Figure 1), the absence of tachycardia, and the relatively short-lived effects of intravascular epinephrine suggest that massive intravascular injection was not the scenario in this patient.(9) In doses used for epidural anesthesia, the beta (2) effects of epinephrine are thought to prevail, resulting in mild reduction of mean arterial blood pressures; however, that was not the situation with this patient. An error of epinephrine dilution is another possibility, although, in retrospect, this has not occurred in our practice. Conclusions A case of a hypertensive parturient who developed a hypertensive crisis after introduction of an epidural block with 2% lidocaine solution containing epinephrine is presented. The pathophysiologic mechanism remains obscure, but a partial intravascular injection through the multiorifice epidural catheter (2) or rapid intravascular absorption are the most likely possibilities. The addition of epinephrine to local anesthetic solutions may offer marginal advantage in quality of analgesia.(3) However, it may pose a possible risk in pre-eclampsia. Lower concentrations of epinephrine can be used in hypertensive parturients without sacrificing the benefits of epinephrine.(4) This case report demonstrates that epinephrine-containing solutions of local anesthetics may place the hypertensive parturient at risk for an hypertensive crisis. REFERENCES: 1. Heller DJ, Goodman C. Use of local anesthetics with epinephrine for epidural anesthesia in preeclampsia. Anesthesiology 1986: 65: 224-226. 2. Gutsche B. Anesthetic considerations for preeclampsia-eclampsia. In: Shnider S. Levinson G. eds. Anesthesia for obstetrics, 2nd ed. Baltimore, Williams and Wilkins, 1979: 224-234. 3. Levy DM. Continuing controversy over use of epidural adrenaline in pre-eclampsia. Br J Hosp Med 1993:49:745. 4. Talledo OK, Chesly LC, Zuspan FP. Reninangiotensin system in normal and toxemic pregnancy. III. Differential sensitivity to angiotensin II and norepinephrine in toxemia of pregnancy. Am J Obstet Gynecol 1968: 100: 218. 5. Robinson DA. Epinephrine should not be used with local anesthetics for epidural anesthesia in preeclampsia. Anesthesiology 1987: 66: 578-579. 6. Dror A, Abboud TK, Moore J. Swart F. Mosaad P. Davis H. Gangolly J. Mantilla M, Makar A, Zaki N. Maternal hemodynamic responses to epinephrinecontaining local anesthetics in mild pre-eclampsia. RegAnesth 1988: 13: 107-111. 7. Birnbach DJ, Stein DJ, Thomas K, Grunebaum A, Thys DM. Cocaine abuse in the parturient: What are the anesthetic implications? Anesthesiology 1993: 79: A988. 8. Cunningham FG, Lindheimer MD. Current concepts: Hypertension in pregnancy. N Engl J Med 1992: 6: 927-932. 9. Takasaki M, Kajitani H. Plasma lidocaine concentrations during continuous epidural infusion of lidocaine with and without epinephrine. Can J Anaesth 1990: 37: 169. 10. Kennedy W, Sawyer TK, Gerbershagen HU, Cutler, RE, Allen GD, Bonica JJ. Systemic cardiovascular and renal hymodynamic alteration during peridural anesthesia in normal man. Anesthesiology 1969:31: 414-421. 11. Murphy TM, Mather LE, Stanton-Hicks MDA, Bonica JJ, Tucker GT. The effects of adding adrenaline to etidocaine and lignocaine in extradural anaesthesia. I: Block characteristics and cardiovascular effects. Br J Anaesth 1976: 48: 893-898. 12. Bonica JJ, Akamatsu TJ, Berges PU, Morikawa K-I, Kennedy WF. Circulatory effects of peridural block. II. Effects of epinephrine. Anesthesiology 1971:34: 514-522. 13. Beck H, Brassow F, Doein M, Bause H, Dziadzka A, Schulte am~sch J. Epidural catheters of the multiorifice type: Dangers and complications. Acta Anaesthesiol Scand 1986: 30: 549-555. 14. Brose WG, Cohen SE. Epidural lidocaine for cesarean section: Effect of varying epinephrine concentration. Anesthesiology 1988: 69: 936-940. |
![[advertisement] gehealthcare](../../../files/banners/banner1_250x600/GEtouch(250X600).gif)






 Educational Material Download
Educational Material Download
Post your comment