Oral and Maxillofacial Regional Anesthesia - continued
|
Maxillary Nerve Block Less often used in clinical practice, the maxillary nerve block (second division block) provides anesthesia of a hemimaxilla. This technique is useful for procedures that require anesthesia of multiple teeth and surrounding buccal and palatal soft tissue in one quadrant or when acute inflammation and infection preclude successful administration of anesthesia by the aforementioned methods. There are two techniques one can use to achieve the maxillary nerve block: the high tuberosity approach and the greater palatine canal approach. The high tuberosity approach carries with it the risk of hematoma formation and is therefore contraindicated in patients with coagulation disorders. The maxillary artery is the vessel of primary concern with the high tuberosity approach. Both techniques are contraindicated when acute inflammation and infection is present over the injection site. High Tuberosity Approach A 25 gauge long needle is preferred for this technique. Technique- The patient should be in the supine position with the chin tilted upward for visibility of the area to be anesthetized. Identify the area to be anesthetized. The right handed operator should be at the ten o'clock position whereas the left handed operator should be at the two o'clock position. This technique anesthetizes the maxillary nerve as it travels through the pterygopalatine fossa. Identify the height of the mucobuccal fold just distal to the maxillary 2nd molar. This is the injection site. The needle should enter the tissue at a forty five degree angle aimed posteriorly, superiorly and medially as in the PSA nerve block (See Fig. 11, B). The bevel should be oriented toward the bone. The needle is advanced to a depth of approximately 30mm or a few millimeters shy of the hub. At this depth, the needle lies within the pterygopalatine fossa. The operator should then aspirate, rotate the needle one quarter turn, and aspirate again. After negative aspiration in two planes has been established, slowly inject one cartridge of anesthetic solution over the course of one minute. The needle is then slowly withdrawn and recapped. Successful administration of anesthetic using this technique provides anesthesia to the entire hemimaxilla on the ipsilateral side of the block. This includes pulpal anesthesia to the maxillary teeth, buccal and palatal soft tissue as far medially as the midline, as well as the skin of the upper lip, lateral aspect of the nose and lower eyelid. Greater Palatine Canal Approach A 25 gauge long needle is preferred for this technique. Technique- Place the patient in the supine position. The right handed operator should be at the ten o'clock position whereas the left handed operator should be at the two o'clock position. Identify the greater palatine foramen as described in the technique for the greater palatine nerve block. The tissue directly over the greater palatine foramen is the target for injection. This technique anesthetizes the maxillary nerve as it travels through the pterygopalatine fossa via the greater palatine canal. Apply pressure to the area over the greater palatine foramen with a cotton tipped applicator. Administer a greater palatine nerve block using the aforementioned technique (See Fig. 14, B). Once adequate palatal anesthesia is achieved, gently probe for the greater palatine foramen with the tip of the needle. For this technique, the syringe should be held so that the needle is aimed posteriorly. It may be necessary to change the angulation of the needle in order to locate the foramen. In a case study performed by Malamed and Trieger, the majority of canals were angled 45-50 degrees. Once the foramen has been located, advance the needle to a depth of 30mm. If resistance is met, withdraw the needle a few millimeters and reenter at a different angle. Malamed and Trieger's study indicates that bony obstructions preventing passage of the needle were found in approximately 5% to 15% of canals. If resistance is met early on and the operator is unable to advance the needle into the canal more than a few millimeters, the procedure should be aborted and the high tuberosity approach should be considered. If no resistance is met and penetration of the canal is successful, aspirate in two planes as described in previous sections and slowly deposit one cartridge of local anesthetic solution. As with the high tuberosity approach, the hemimaxilla on the ipsilateral side as the injection becomes anesthetized with successful execution of this technique.1,6,7 Intraseptal Injection The intraseptal technique is a useful adjunct to the aforementioned techniques (supraperiosteal, PSA, MSA, ASA). Although not used as often in clinical practice, the technique is very similar to the PDL injection and offers the added advantage of hemostasis in the area of injection. Terminal nerve endings in the surrounding hard and soft tissue of individual teeth are anesthetized with this technique. Contraindications to the procedure include acute inflammation and infection over the site of injection. A 27 gauge short needle is preferred for this technique. Technique- Place the patient in the supine position. The target area is the interdental palpillae 2-3mm apical to the apex of the papillary triangle (Fig. 17). The right handed operator should be at the ten o'clock position whereas the left handed operator should be at the two o'clock position. The operator may ask the patient to turn his or her head for optimum visibility. The syringe is held at a 45 degree angle to the long axis of the tooth with the bevel facing the apex of the root. The needle is inserted into the soft tissue and is advanced until bone is contacted. A few drops of anesthetic should be administered at this time. The needle is then advanced into the interdental septum and 0.2cc of anesthetic solution is deposited. Resistance to the flow of anesthetic solution is expected and ischemia of the soft tissue surrounding the injection site will ensue shortly after anesthetic solution is administered.1 
Figure 17: Note the position of the needle 3mm apical to the apex of the papillary triangle for the intraseptal technique. Clinical Pearls
Techniques of Mandibular Regional Anesthesia Techniques used in clinical practice for the anesthesia of the hard and soft tissues of the mandible include the supraperiosteal technique, PDL injection, intrapulpal anesthesia, intraseptal injection, inferior alveolar nerve block, long buccal nerve block, Gow-Gates technique, Vazirani-Akinosi closed mouth mandibular block, mental nerve block, and incisive nerve block. The supraperiosteal, PDL, intrapulpal, and intraseptal techniques are executed in the same manner as described above for maxillary anesthesia. When anesthetizing the mandible the patient should be in the semisupine or reclined position. The right handed operator should stand at the nine o'clock to ten o'clock position whereas the left handed operator should stand at the three o'clock to four o' clock position. Inferior Alveolar Nerve Block The inferior alveolar nerve block is one of the most commonly employed techniques in mandibular regional anesthesia. It is extremely useful when multiple teeth in one quadrant require treatment. While effective, this technique carries a high failure rate even when strict adherence to protocol is maintained. The target for this technique is the mandibular nerve as it travels on the medial aspect of the ramus, prior to its entry into the mandibular foramen. The lingual, mental, and incisive nerves are also anesthetized. A 25 gauge long needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. With the mouth open maximally, identify the coronoid notch and the pterygomandibular raphae. Three quarters of the anteroposterior distance between these two landmarks, and approximately six to ten millimeters above the occlusal plane is the injection site. Use a retraction instrument to retract the cheek and bring the needle to the injection site from the contralateral premolar region. As the needle passes through the soft tissue, deposit one or two drops of anesthetic solution. Advance the needle until bone is contacted. Once bone is contacted, withdraw the needle one millimeter and redirect the needle posteriorly by bringing the barrel of the syringe towards the occlusal plane (Fig. 18, A and B). Advance the needle to three quarters of its depth, aspirate, and inject three quarters of a cartridge of anesthetic solution slowly over the course of one minute. As the needle is withdrawn, continue to deposit the remaining one quarter of anesthetic solution so as to anesthetize the lingual nerve (Fig. 18, C). Successful execution of this technique results in anesthesia of the mandibular teeth on the ipsilateral side to the midline, associated buccal and lingual soft tissue, lateral aspect of the tongue on the ipsilateral side, and lower lip on the ipsilateral side.1 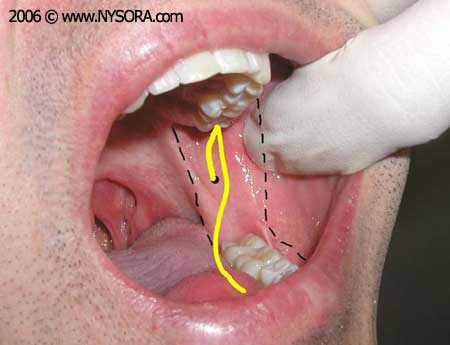
Figure 18A: Location of the inferior alveolar nerve. 
Figure 18B: After contacting bone, the needle is redirected posteriorly by bringing the barrel of the syringe towards the occlusal plane. The needle is then advanced to three quarters of its depth. 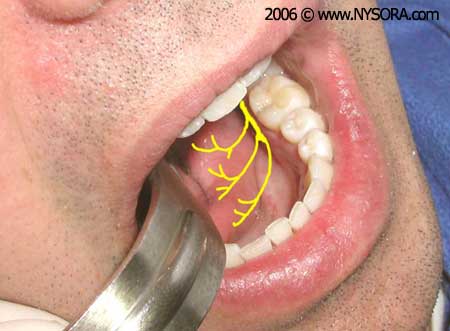
Figure 18C: Location of the lingual nerve which is anesthetized during the administration of an inferior alveolar nerve block. Buccal Nerve Block The buccal nerve block, otherwise known as the long buccal or buccinator block, is a useful adjunct to the inferior alveolar nerve block when manipulation of the buccal soft tissue in the mandibular molar region is indicated. The target for this technique is the buccal nerve as it passes over the anterior aspect of the ramus. Contraindications to the procedure include acute inflammation and infection over the site of injection. A 25 gauge long needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. Identify the most distal molar tooth on the side to be treated. The tissue just distal and buccal to the last molar tooth is the target area for injection (Fig. 19, A and B). Use a retraction instrument to retract the cheek. The bevel of the needle should be toward bone and the syringe should be held parallel to the occlusal plane on the side of the injection. The needle is inserted into the soft tissue and a few drops of anesthetic solution are administered. The needle is advanced approximately one or two millimeters until bone is contacted. Once bone is contacted and aspiration is negative, 0.2cc of local anesthetic solution is deposited. The needle is withdrawn and recapped. Successful execution of this technique results in anesthesia of the buccal soft tissue of the mandibular molar region.1 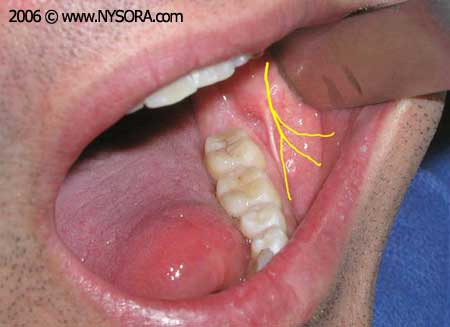
Figure 19A: Location of the buccal nerve. 
Figure 19B: The tissue just distal and buccal to the last molar tooth is the target area for injection. Gow-Gates Technique The Gow-Gates technique or third division nerve block is useful alternative to the inferior alveolar nerve block and is often used when the latter fails to provide adequate anesthesia. Advantages of this technique versus the inferior alveolar technique are its low failure rate and low incidence of positive aspiration. The Gow-Gates technique anesthetizes the auriculotemporal, inferior alveolar, buccal, mental, incisive, mylohyoid and lingual nerves. Contraindications to this procedure include acute inflammation and infection over the site of injection and trismatic patients. A 25 gauge long needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. The target area for this technique is the neck of the condyle below the area of insertion of the lateral pterygoid muscle. A retraction instrument is used to retract the cheek. The patient is asked to open maximally and the mesiolingual cusp of the maxillary 2nd molar on the side of desired anesthesia is identified. The insertion site of the needle will be just distal to the maxillary 2nd molar at the level of the mesiolingual cusp. Bring the needle to the insertion site in a plane that is parallel to an imaginary line drawn from the intertragic notch to the corner of the mouth on the same side as the injection (Fig. 20, A and B). The orientation of the bevel of the needle is not important in this technique. Advance the needle through soft tissue approximately 25mm until bone is contacted. This is the neck of the condyle. Once bone is contacted, withdraw the needle one millimeter and aspirate. Redirect the needle superiorly and reaspirate. If aspiration in two planes is negative, slowly inject one cartridge of local anesthetic solution over the course of one minute. Successful execution of this technique provides anesthesia to the ipsilateral mandibular teeth up to the midline, and associated buccal and lingual hard and soft tissue. The anterior two thirds of the tongue, floor of the mouth, skin over the zygoma, posterior aspect of the cheek and temporal region on the ipsilateral side of injection are also anesthetized.1,8 
Figure 20A: The patient is asked to open mouth maximally. The mesiolingual cusp of the maxillary 2nd molar is the reference point for the height of the injection. 
Figure 20B: The needle is then moved distally and is held parallel to an imaginary line drawn from the intertragic notch to the corner of the mouth. Vazirani-Akinosi Closed Mouth Mandibular Block The Vazirani-Akinosi closed mouth mandibular block is a useful technique for patients with limited opening due trismus or ankylosis of the temporomandibular joint. Limited mandibular opening precludes the administration of the inferior alveolar nerve block or use of the Gow-Gates technique both of which require the patient to be open maximally. Other advantages to this technique are the minimal risk of trauma to the inferior alveolar nerve, artery, vein, and pterygoid muscle, low complication rate and minimal discomfort upon injection. Contraindications to this technique are acute inflammation and infection in the pterygomandibular space, deformity or tumor in the maxillary tuberosity region or an inability to visualize the medial aspect of the ramus. A 25 gauge long needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. The gingival margin above the maxillary 2nd and 3rd molars and the pterygomandibular raphae serve as landmarks for this technique. A retraction instrument is used to stretch the cheek laterally. The patient should occlude gently on the posterior teeth. The needle is held parallel to the occlusal plane at the level of the gingival margin of the maxillary 2nd and 3rd molars. The bevel is directed away from the bone facing the midline. The needle is advanced through the mucous membrane and buccinator muscle to enter the pterygomandibular space. The needle is inserted to approximately one half to three quarters of its length. At this point the needle will be in the midsection of the ptyerygomandibular space. Aspirate and if negative, one cartridge of local anesthetic solution is deposited over the course of one minute. Diffusion and gravitation of the local anesthetic solution will anesthetize the lingual and long buccal nerves in addition to the inferior alveolar nerve. Successful execution of this technique provides anesthesia of the ipsilateral mandibular teeth up to the midline, and associated buccal and lingual hard and soft tissue. The anterior two thirds of the tongue and floor of the mouth are also anesthetized.9,10 Mental Nerve Block The mental nerve block is indicated for procedures where manipulation of buccal soft tissue anterior to the mental foramen is necessary. Contraindications to this technique are acute inflammation and infection over the injection site. A 25 or 27 gauge short needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. The target area is the height of the mucobuccal fold over the mental foramen (Fig. 21, A and B). The foramen can be manually palpated by applying gentle finger pressure to the body of the mandible in the area of the premolar apicies. The patient will feel slight discomfort upon palpation of the foramen. Use a retraction instrument to retract the soft tissue. The needle is directed toward the mental foramen with the bevel facing the bone. Penetrate the soft tissue to a depth of five millimeters, aspirate and inject approximately 0.6cc of anesthetic solution. Successful execution of this technique results in anesthesia of the buccal soft tissue anterior to the foramen, lower lip and chin on the side of the injection.1 
Figure 21A: Location of the mental and incisive nerves. 
Figure 21B: Block of the mental and incisive nerves: The needle is inserted at the height of the mucobuccal fold over the mental foramen for both the mental nerve block and incisive nerve block. Incisive Nerve Block The incisive nerve block is not as frequently employed in clinical practice however it proves very useful when treatment is limited to mandibular anterior teeth and full quadrant anesthesia is not necessary. The technique is almost identical to the mental nerve block with one additional step. Both the mental and incisive nerves are anesthetized using this technique. Contraindications to this technique are acute inflammation and infection at the site of injection. A 25 or 27 gauge short needle is preferred for this technique. Technique- The patient should be in the semisupine position. The right handed operator should be in the eight o'clock position whereas the left handed operator should be in the four o'clock position. The target area is the height of the mucobuccal fold over the mental foramen (See Fig. 21, B). Identify the mental foramen as previously described. Give the patient a mental nerve block as described above and apply digital pressure at the site of injection during administration of anesthetic solution. Continue to apply digital pressure at the site of injection two to three minutes after the injection is complete to aid the anesthetic in diffusing into the foramen. Successful implementation of this technique provides anesthesia to the premolars, canine, incisor teeth, lower lip, skin of the chin, and buccal soft tissue anterior to the mental foramen.1 REFERENCES: 1. Malamed, SF Handbook of Local Anesthesia, 4th Edition 1997, Mosby-Year Book Inc. 2. Snell, RS Clinical Anatomy for Medical Students, 5th Edition 1995, Little, Brown and Company Inc. 3. Loestscher CA, and Walton RE Patterns of Innervation of the Maxillary First Molar: A Dissection Study Oral Surgery Oral Medicine Oral Pathology 65: 86-90, 1988 4. McDaniel, WM Variations in Nerve Distributions of the Maxillary Teeth Journal of Dental Research 35: 916-921, 1956 5. Heasman PA, Clinical Anatomy of the Superior Alveolar Nerves British Journal of Oral and Maxillofacial Surgery 22: 439-447, 1884 6. Malamed SF and Trieger N Intraoral Maxillary Nerve Block: an Anatomical and Clinical Study Anesthesia Progress 30: 44-48, 1983 7. Poore, TE and Carney F Maxillary Nerve Block: A Useful Technique Journal of Oral Surgery 31: 749-755, 1973 8. Gow-Gates, GAE Mandibular Conduction Anesthesia: a New Technique Using Extraoral Landmarks Oral Surgery 36: 321-328, 1973 9. Akinosi JO, A New Approach to the Mandibular Nerve Block British Journal of Oral and Maxillofacial Surgery 15: 83-87, 1977 10. Vazirani, SJ, Closed Mouth Mandibular Nerve Block: A New Technique Dental Digest 66: 10-13, 1960 |
||||||||||||||||||||||||||||||||
![[advertisement] gehealthcare](files/banners/banner1_250x600/GEtouch(250X600).gif)







 Educational Material Download
Educational Material Download



































Post your comment